Bronchospasm treatment: August 2023 updates and what patients should know
If you had tightness in your chest or sudden wheeze this month, the posts from August 2023 focused on what’s changing in bronchospasm care. The main article walks through new research, promising drugs, and practical steps you can take now. I’ll give you the highlights and simple things to discuss with your clinician.
What’s changing in treatment
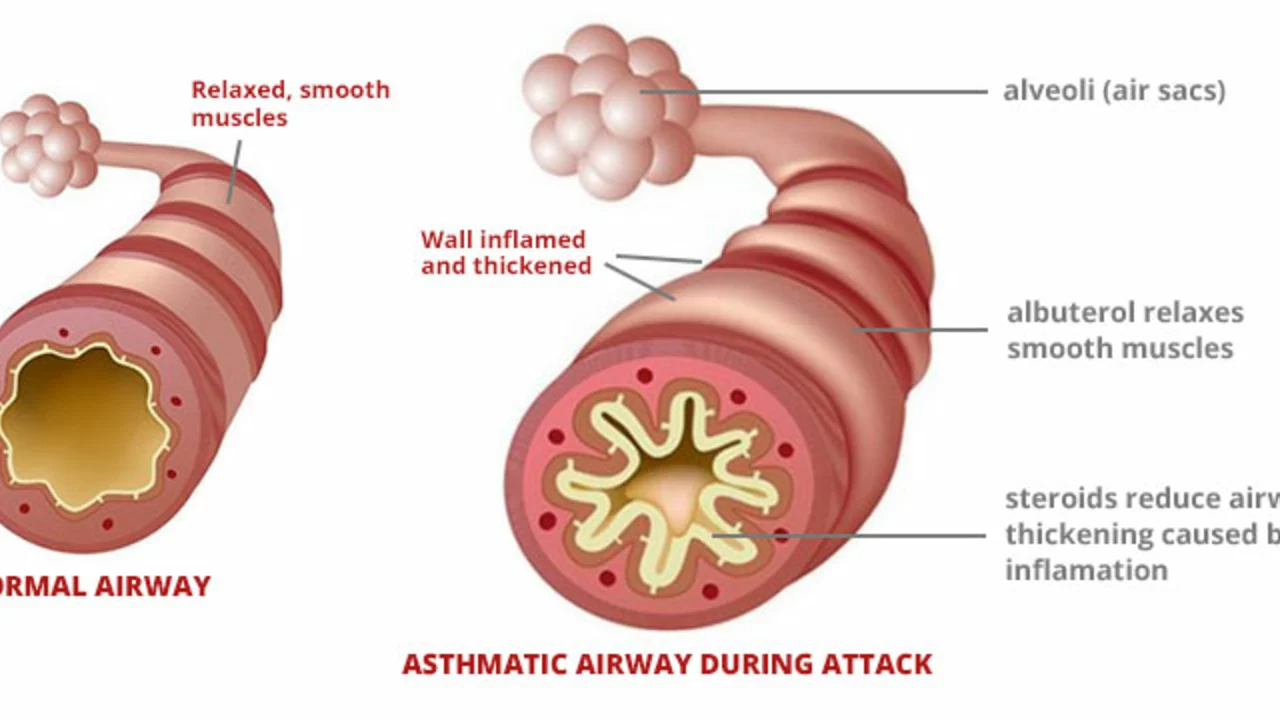
Research has shifted from just symptom relief to targeting the causes behind bronchospasm. For people with severe asthma, biologic drugs that target specific immune signals (like IL-5, IL-4/13, or IgE) are already helping those with certain blood markers. These aren’t for everyone, but if you have frequent flare-ups despite inhalers, ask a specialist whether testing for biologic eligibility makes sense.
Long-acting bronchodilators and combination inhalers continue to improve. Newer inhaler mixes combine a long-acting beta-agonist with an antimuscarinic and a steroid to give steadier control and fewer daily doses. That often means fewer sudden spasms for many people, especially when used correctly.
Device tech is getting smarter. Devices that track inhaler use, record symptoms, or remind you to take medication help with real-world adherence — and missing doses is a common reason symptoms get worse. Nebulizer formulations and faster-onset inhaled drugs are also being tested to give relief quicker during severe episodes.
Practical steps you can take today
First: check your inhaler technique. Even the best medicine won’t work if it’s not delivered properly. Ask your nurse or pharmacist to watch you use it and correct your technique. Use a spacer with an MDI if instructed — that cuts down on throat side effects and gets more drug to the lungs.
Second: track triggers and symptoms. Write down what comes before a flare — pollen, cold air, exercise, or an irritant at work. Triggers help your doctor tailor treatment and may point to avoidance strategies that cut episodes down.
Third: talk about advanced options only if you need them. If you’re relying on rescue inhalers more than twice a week or have frequent night symptoms, bring that up. Tests like blood eosinophil counts or FeNO can clarify whether biologics or other advanced therapies might help.
Fourth: keep an action plan and know when to get urgent help. If rescue meds don’t ease breathing, or you have fast breathing, blue lips, or struggle to speak, seek emergency care.
August’s coverage is practical: it doesn’t promise a cure, but it shows clearer paths for people whose bronchospasm isn’t controlled. Read the full post in this archive for examples, device tips, and how to prepare questions for your clinician. If you want, subscribe or save this page so you can revisit the specifics when you talk with your healthcare team.