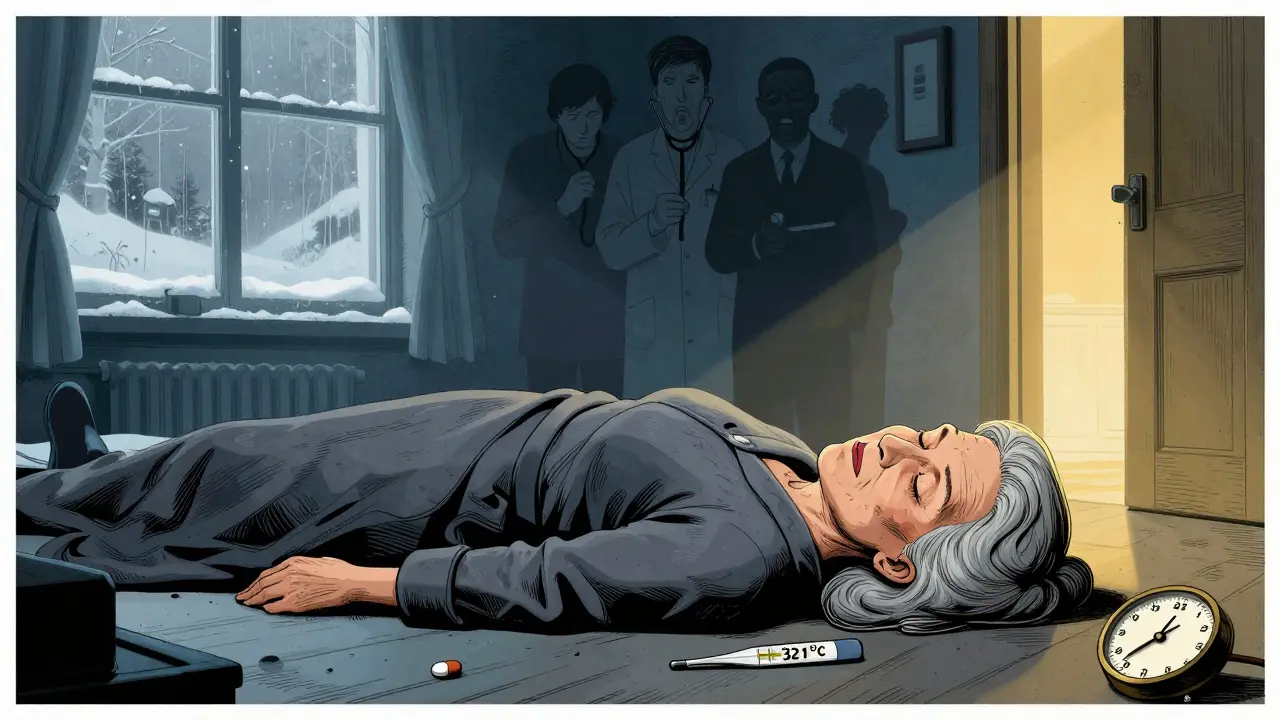
Myxedema coma isn’t just a rare complication of hypothyroidism-it’s a ticking time bomb. Every hour without treatment raises the risk of death by 10%. And yet, many patients are misdiagnosed for months, their symptoms written off as aging, depression, or just being "lazy." This isn’t theoretical. In Melbourne, a 72-year-old woman was admitted to the ER after her family found her unresponsive in a cold house during winter. Her temperature was 32.1°C. Her heart rate was 38 beats per minute. Her sodium was 128. She hadn’t taken her thyroid medication in six weeks. She survived-because someone finally suspected myxedema coma. Too many don’t.
What Exactly Is Myxedema Coma?
Myxedema coma, now more accurately called myxedema crisis, is the body’s final collapse under years of untreated or poorly managed hypothyroidism. It doesn’t happen overnight. It builds slowly: fatigue that gets worse, weight gain that won’t budge, cold intolerance that turns into shivering even indoors. Then, something triggers the crash-a pneumonia, a missed dose, a cold snap, a hospital stay where meds were stopped. That’s when the brain slows, the heart stumbles, and the body stops regulating itself.It’s not about feeling tired. It’s about your core temperature dropping below 35°C. Your breathing slowing to under 12 breaths a minute. Your sodium levels crashing. Your heart rate dropping so low your blood pressure follows. You may not even be conscious. And yes, you can have this without being in a full coma. The old term "coma" is misleading. The real danger is multi-organ failure from zero thyroid hormone.
Most cases happen in women over 60. But men get it too-and they’re more likely to be missed because doctors don’t expect it. One study found men waited 40% longer for diagnosis. That’s deadly.
The Classic Signs (And the Sneaky Ones)
There’s a triad doctors look for: altered mental status, hypothermia, and a triggering event. But here’s what doesn’t show up on a checklist:- Profound lethargy-not just sleepy, but unable to speak or move without effort. Reported in 98% of cases.
- Non-pitting edema-swelling in the face, eyelids, lips. Not like water retention you can press and leave a dent. This is thick, doughy, and doesn’t budge.
- Respiratory failure-low oxygen, high carbon dioxide. Patients don’t gasp. They just stop breathing deeply. Many need intubation.
- Ileus-the gut shuts down. No bowel movements for days. No hunger. No nausea. Just silence.
- Hyponatremia-sodium below 135. Often below 125. This isn’t just a lab number. It’s brain swelling waiting to happen.
And here’s the kicker: 30% of elderly patients show up with "apathetic hypothyroidism." No weight gain. No dry skin. No hair loss. Just confusion, falls, and a slow decline. If you see an older person with unexplained confusion and low body temperature-think thyroid. Now.
Why Time Is the Enemy
Mortality? Between 25% and 60%. That’s not a typo. Even with modern ICU care, nearly half don’t make it. Why? Delay.On average, patients wait 6 to 12 hours from first suspicion to treatment. That’s too long. Every hour without thyroid hormone increases death risk by 10%. The American Thyroid Association says: don’t wait for labs. Start treatment the moment you suspect it.
Think of it like a car running on fumes. The engine sputters. The lights dim. You don’t wait for the fuel gauge to hit zero before you refill. You refill before it dies. Same here. If the clinical picture fits, give the hormone. Now.

Emergency Protocol: What to Do, Step by Step
There’s a clear, evidence-backed sequence. Skip a step, and you risk killing the patient.- Secure the airway. If the patient is lethargic, slow-breathing, or has high CO2, intubate. Don’t wait. Respiratory arrest is common.
- Give thyroid hormone immediately. IV levothyroxine (T4): 300-500 mcg loading dose. Then 50-100 mcg daily. In severe cases-especially with heart problems-add liothyronine (T3): 10-20 mcg every 8 hours. New guidelines now recommend T3 first in cardiac compromise.
- Warm slowly. No heating blankets. No warm baths. Passive rewarming only. Active warming causes blood vessels to dilate too fast. The heart can’t handle it without hormone support. Monitor core temp every 30 minutes.
- Treat the trigger. Infection? Start broad-spectrum antibiotics now. Pneumonia? UTI? Sepsis? 50% of cases are triggered by infection. Don’t wait for cultures. Cover gram-positive and gram-negative bugs.
- Correct sodium carefully. Don’t rush. Raise sodium by no more than 4-6 mmol/L in 24 hours. Too fast? You risk central pontine myelinolysis-a brain injury that can leave patients locked-in.
Use the DIMES mnemonic to spot triggers: Drugs (like sedatives or opioids), Infection, Myocardial infarction or stroke, Exposure to cold, Stroke. Check for all five.
What Doesn’t Work (And Why)
Many well-intentioned actions make things worse.- Glucocorticoids alone. Some give hydrocortisone thinking it’s adrenal crisis. It helps if adrenal insufficiency is suspected, but it doesn’t replace thyroid hormone. Don’t use it as a substitute.
- Oral thyroid meds. If the gut’s shut down (ileus), oral T4 won’t absorb. IV is non-negotiable.
- Aggressive fluid resuscitation. Patients often have fluid overload already. Too much IV fluid worsens hyponatremia and heart strain.
- Waiting for TSH results. TSH can take hours. By then, it’s too late. Clinical suspicion is the only test that matters at this stage.
One ER doctor in Sydney told me: "I once held off on T4 because the TSH was pending. The patient coded 45 minutes later. The result came back at 147 mIU/L. I’ll never wait again."
Who’s at Risk-and Why It’s Getting Worse
Myxedema coma affects 0.2 to 0.6 people per million each year. But in those over 60? That jumps to 4-6 per million. And it’s rising.Why? Aging populations. More people on long-term thyroid meds. More hospitalizations where meds get stopped. More cold winters. More undiagnosed hypothyroidism in low-resource areas.
And here’s the hidden crisis: uninsured patients wait 35% longer for treatment and die 22% more often. In Australia, even with Medicare, patients in rural areas often don’t get timely blood tests. A woman in regional Victoria waited 11 days after her GP dismissed her symptoms as "just menopause." She ended up in ICU. She survived. But she’ll never walk the same again.
Research from 2023 shows that elevated thyrotropin receptor antibodies can predict who’s about to crash-before they collapse. Point-of-care thyroid tests are in trials and promise results in 15 minutes. That could save thousands.
What Patients and Families Should Know
If you have hypothyroidism:- Never stop your meds without a doctor’s order-even for a short hospital stay.
- If you’re feeling unusually sluggish, cold, confused, or swollen, say so. Loudly.
- Keep a list of your meds and doses with you at all times.
- If you’re elderly and have unexplained confusion or falls, ask: "Could this be my thyroid?"
Family members are often the first to notice. A daughter told me: "Mom used to make tea every morning. Then she stopped. She just sat in her chair, staring. She didn’t answer when I spoke. I thought she was getting dementia. I didn’t know thyroid could do this."
Early recognition saves lives. And it’s not complicated. Low temp. Slow heart. Low sodium. Mental fog. Thyroid meds not taken? That’s the signal.
Final Thought: This Is Preventable
Myxedema coma isn’t a mystery. It’s a failure of vigilance. We know the signs. We know the protocol. We know the risks. The gap isn’t in knowledge-it’s in action.Doctors need to stop dismissing fatigue in older women as "just aging." Families need to speak up when something feels "off." And patients need to know: your thyroid isn’t just about weight or energy. It’s about survival.
The next time someone says, "She’s just getting old," ask: "What if she’s dying-and we can stop it?"
Can myxedema coma happen without a known history of hypothyroidism?
Yes. About 20-30% of cases occur in people who never had a formal diagnosis. Symptoms like fatigue, cold intolerance, and constipation were ignored or misattributed to aging, depression, or chronic illness. By the time they collapse, the thyroid has been failing for years. This is why unexplained hypothermia and altered mental status in older adults must always trigger a thyroid test-even without prior history.
Why can’t we just give oral thyroid medication?
In myxedema coma, the gut often shuts down (ileus), so oral meds won’t absorb. Even if absorbed, the body can’t convert T4 to active T3 efficiently without proper metabolic function. IV levothyroxine delivers the hormone directly into the bloodstream, and adding IV liothyronine (T3) gives immediate active hormone to the brain and heart. Oral pills are too slow and unreliable in this emergency.
Is myxedema coma the same as thyroid storm?
No. They’re opposites. Thyroid storm is caused by too much thyroid hormone-leading to fever, rapid heartbeat, high blood pressure, and agitation. Myxedema coma is caused by too little-leading to low temperature, slow heart rate, low blood pressure, and lethargy. Treatment is the opposite: antithyroid drugs for storm, hormone replacement for coma. Confusing them can be fatal.
Why is passive rewarming recommended instead of active warming?
Active warming (heating blankets, warm IV fluids) causes blood vessels to dilate rapidly. Without sufficient thyroid hormone, the heart can’t pump enough blood to meet the increased demand. This can trigger cardiac arrest. Passive rewarming-using blankets, warm rooms, and body heat-lets the body warm gradually, giving the heart time to adjust once hormone levels start rising.
How quickly should someone improve after treatment?
Improvement often begins within 24 to 48 hours. Mental status improves first-patients become more alert, responsive. Heart rate and temperature follow. Full recovery can take days to weeks, depending on how long the body was without hormone support. But if there’s no sign of improvement after 48 hours, check for other problems: infection, kidney failure, or missed triggers.
Can myxedema coma recur?
Yes, if thyroid hormone replacement isn’t properly managed after recovery. Patients need lifelong thyroid medication and regular monitoring. Missing doses, stopping meds during illness, or not adjusting doses after hospitalization can lead to another crisis. Education and medication adherence are critical for long-term survival.

Hilary Miller
January 22, 2026 AT 22:53My aunt went through this. No one believed her until she stopped answering calls. Then it was too late.
Oren Prettyman
January 24, 2026 AT 16:01While I appreciate the clinical detail, the framing here feels alarmist. Myxedema coma is statistically negligible compared to the millions of patients who manage hypothyroidism without incident. The 10% mortality-per-hour statistic is misleading without context-this only applies to the vanishingly small subset who’ve gone completely untreated for months while ignoring all signs. It’s not a ticking time bomb; it’s a consequence of systemic neglect, not inherent disease progression. We’re conflating failure of care with inevitability of collapse.
Tatiana Bandurina
January 25, 2026 AT 17:07Let’s be honest-this is what happens when you let elderly women go undiagnosed because doctors are too lazy to order TSH. I’ve seen it in my mother’s nursing home. Nurses say ‘she’s just tired’ for weeks. Then one day she’s cold and silent. No one checks thyroid levels until someone screams. It’s not about knowledge. It’s about who they think is worth saving.
Philip House
January 25, 2026 AT 17:43Look, I get it. Thyroid stuff is important. But let’s not pretend this is some hidden epidemic. Most people who miss their meds just feel sluggish for a few weeks and then remember. This is the rarest of rare cases. The real problem is overtesting. Every grandma with low energy gets a full thyroid panel now. It’s driving up costs and scaring people into thinking they’re one missed pill from dying. Chill out. The body’s got reserves.
Sarvesh CK
January 27, 2026 AT 03:49It is both tragic and instructive that such a preventable condition continues to claim lives in the modern era. The medical literature is unequivocal, yet human systems-fueled by cognitive biases, time constraints, and implicit ageism-fail to act. The case of the woman in rural Victoria is emblematic: a societal disregard for the silent suffering of the elderly, particularly women, masks itself as benign neglect. We must recognize that medical knowledge without cultural vigilance is inert. Education must extend beyond clinicians to families, caregivers, and community health workers. Point-of-care testing, as mentioned, is not merely a technological advancement-it is an ethical imperative.
Malik Ronquillo
January 28, 2026 AT 08:13Why do doctors always wait for labs? I’ve seen this too. My neighbor’s dad died because they waited for TSH. He was in his 70s, sat in a chair for days, didn’t eat. They called it dementia. He wasn’t dementia. He was dying. And now he’s gone. Just give the damn pills. No one dies from giving T4 too early. But people die from waiting.
Chiraghuddin Qureshi
January 28, 2026 AT 19:43So true 😔 I saw this in my uncle in Delhi-he stopped taking his medicine during a hospital stay for pneumonia. They didn’t check his thyroid. He was found curled up on the floor. Took 3 days to get T4. He survived but lost 15kg and can’t walk stairs now. #ThyroidAwareness
Ryan Riesterer
January 28, 2026 AT 22:48Passive rewarming is physiologically sound: catecholamine depletion in hypothyroidism impairs vasoconstrictive response, making active external warming a risk for afterdrop and arrhythmia. The 2012 ATA guidelines reinforce this, and recent ICU studies (e.g., JCEM 2021) show improved survival with normothermic rewarming protocols. IV T4 + T3 remains gold standard, but T3 dosing should be titrated by cardiac status-especially in those with prior MI. The key insight: this isn’t endocrinology. It’s critical care with a thyroid etiology.