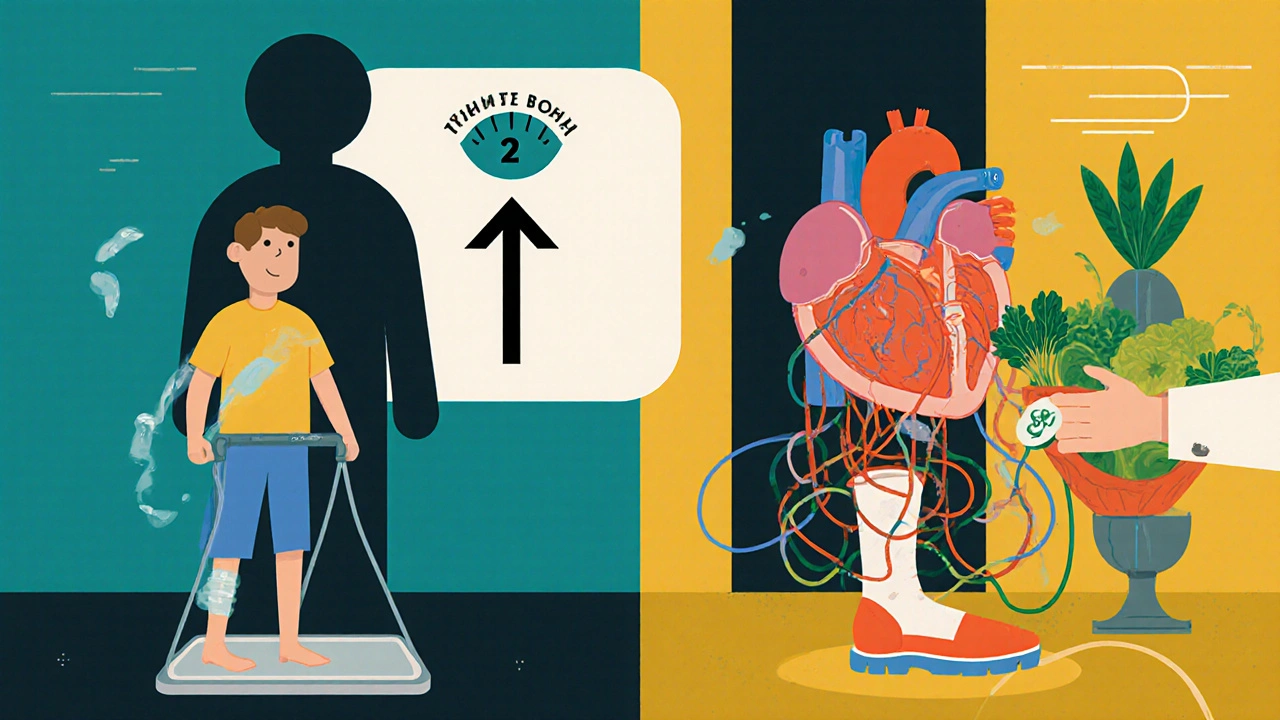
If you’re living with congestive heart failure, what you eat isn’t just about feeling good-it’s about keeping your heart from working harder than it already is. The wrong foods can make symptoms worse, send you back to the hospital, or speed up the disease. The good news? Simple, clear changes to your diet can help you breathe easier, reduce swelling, and feel more like yourself.
Why Diet Matters in Congestive Heart Failure
Congestive heart failure means your heart can’t pump blood as well as it should. That causes fluid to build up in your lungs, legs, and belly. Salt and too much fluid make this worse. Your heart has to push harder to move blood through swollen vessels, and over time, that extra strain wears it down even more.
Studies show that people who follow a strict low-sodium diet and manage fluid intake have fewer hospital visits and better quality of life. In fact, one 2023 review of 12 clinical trials found that patients who stuck to under 2,000 mg of sodium per day reduced their risk of heart failure hospitalization by nearly 40% compared to those who didn’t.
The Two Biggest Rules: Sodium and Fluids
These are not suggestions. They’re medical necessities.
Sodium (salt): Most people eat over 3,500 mg of sodium a day. For heart failure patients, the goal is usually under 2,000 mg-sometimes as low as 1,500 mg. That’s less than a teaspoon of table salt. But salt doesn’t just come from the shaker. It’s hidden in bread, canned soups, deli meats, frozen meals, and even breakfast cereals.
Fluids: Many doctors recommend limiting fluids to 1.5 to 2 liters (about 6 to 8 cups) per day. This includes water, juice, coffee, soup, ice cream, and even gelatin. Why? Because your heart can’t handle the extra volume. Too much fluid means more pressure on your heart and lungs, leading to shortness of breath and swelling.
Keep a daily log. Write down everything you drink and eat. Use a measuring cup. It’s easy to underestimate how much you’re taking in.
What to Eat: Heart-Friendly Foods
You don’t have to eat bland food. You just need to choose smarter options.
- Fresh vegetables and fruits: Broccoli, spinach, carrots, apples, berries, and oranges are naturally low in sodium and rich in potassium and magnesium-minerals that help balance fluids and support heart rhythm.
- Whole grains: Brown rice, quinoa, oats, and whole wheat pasta give you fiber without added salt. Avoid instant oatmeal or flavored rice mixes-they often have sodium hidden in seasoning.
- Lean proteins: Skinless chicken, turkey, fish (especially salmon, mackerel, sardines), eggs, tofu, and legumes. Avoid smoked, cured, or processed meats like bacon, ham, sausages, and salami. These are loaded with sodium and preservatives.
- Healthy fats: Olive oil, avocado, nuts (unsalted), and seeds. These help reduce inflammation and support blood vessel health.
- Dairy: Choose low-fat or fat-free milk, yogurt, and cheese. Check labels. Some cheeses, like cheddar and feta, are high in sodium. Look for "no salt added" versions.
When cooking, skip the salt. Use herbs and spices instead: garlic, rosemary, thyme, cumin, paprika, lemon juice, and vinegar add flavor without sodium.
What to Avoid: Hidden Traps
Some foods look healthy but are heart failure traps.
- Processed snacks: Chips, pretzels, crackers, and popcorn often have more sodium than you think. Even "low-fat" versions can be high in salt.
- Canned and packaged foods: Canned soups, beans, vegetables, and sauces are loaded with sodium. Look for "no salt added" or rinse canned beans and veggies under water to remove up to 40% of the salt.
- Restaurant meals: A single serving of pasta at a chain restaurant can have over 2,500 mg of sodium. Ask for sauces on the side, skip the cheese, and avoid anything labeled "seasoned," "marinated," or "crispy."
- Condiments: Soy sauce, ketchup, mustard, and salad dressings are sodium bombs. Use small amounts or find low-sodium versions.
- Alcohol: Too much alcohol weakens the heart muscle. Most doctors recommend no more than one drink a day for women and two for men-if at all. Some patients are told to avoid it completely.
Monitoring Your Body’s Signals
Your body will tell you if you’re eating right-or not.
Check your weight every morning, right after using the bathroom and before eating or drinking. A sudden gain of 2 pounds (1 kg) in one day or 5 pounds (2.3 kg) in a week means you’re holding onto fluid. Call your doctor. Don’t wait.
Watch for swelling in your ankles, legs, or belly. If your rings feel tight or your clothes are suddenly snug, that’s a red flag. Shortness of breath that’s worse than usual, especially when lying flat, means your heart is struggling.
Keep a symptom journal. Note your weight, how you feel, what you ate, and how much you drank. Bring it to your next appointment. It helps your doctor adjust your treatment.
Working With Your Care Team
Diet alone isn’t enough. You need to work with your doctor, pharmacist, and a registered dietitian who knows heart failure.
Your medications-like diuretics (water pills)-work best when your diet is on track. But some drugs, like ACE inhibitors or ARBs, can raise potassium levels. That’s why eating too many high-potassium foods like bananas, oranges, potatoes, or spinach might be risky if you’re on those meds. Your doctor will tell you what’s safe.
A dietitian can help you plan meals that fit your taste, budget, and lifestyle. They can show you how to read food labels, swap ingredients, and cook meals that don’t feel like punishment.
Real-Life Examples That Work
Here’s what a day of eating might look like for someone with heart failure:
- Breakfast: Oatmeal made with water, topped with sliced strawberries and a sprinkle of chia seeds. Black coffee (half a cup).
- Lunch: Grilled chicken salad with mixed greens, cherry tomatoes, cucumbers, and olive oil and vinegar dressing. One small whole wheat roll.
- Snack: Unsalted almonds (10-12) and a small apple.
- Dinner: Baked salmon with roasted zucchini and quinoa. A cup of herbal tea.
- Fluids: Water, herbal tea, and a small glass of diluted cranberry juice-total under 1.8 liters.
This meal plan has about 1,400 mg of sodium and stays under fluid limits. It’s simple, tasty, and sustainable.

What If You Slip Up?
Everyone has off days. Maybe you ate a slice of pizza at a family gathering. Maybe you forgot to check the sodium on a canned soup.
Don’t panic. Don’t guilt-trip yourself. Just get back on track the next meal. One high-sodium meal won’t ruin your progress-but if it becomes a habit, it will.
Use slip-ups as learning moments. Ask yourself: What triggered it? Was it stress? Lack of planning? Eating out? Then plan ahead next time. Keep low-sodium snacks on hand. Prep meals on weekends. Keep a list of safe restaurants nearby.
Long-Term Success Comes From Routine
Changing your diet isn’t a short-term fix. It’s a lifelong habit. The more you do it, the easier it gets. Your taste buds adapt. You start to notice how salty most food really is. You’ll feel better, sleep better, and have more energy.
It’s not about perfection. It’s about consistency. Small steps every day add up.
Can I still eat out with congestive heart failure?
Yes, but you need to be smart. Choose grilled, steamed, or baked options. Ask for sauces and dressings on the side. Avoid anything fried, breaded, or seasoned with salt. Request no added salt when ordering. Many restaurants now list sodium content online-check the menu before you go.
Is sea salt better than table salt for heart failure?
No. Sea salt, kosher salt, Himalayan salt-they’re all sodium chloride. The mineral content might be slightly different, but the sodium amount is nearly the same. One teaspoon of any salt has about 2,300 mg of sodium. The idea that sea salt is healthier is a myth.
Can I use salt substitutes?
Be careful. Many salt substitutes replace sodium with potassium. If you’re taking certain heart medications like ACE inhibitors or potassium-sparing diuretics, extra potassium can be dangerous and cause irregular heart rhythms. Always talk to your doctor before using them.
How much water should I drink each day?
Most heart failure patients are advised to limit total fluids to 1.5 to 2 liters per day. This includes water, tea, coffee, juice, soup, ice cream, and even foods that melt at room temperature. Your doctor will give you a specific number based on your condition. Use a marked water bottle to track intake.
Do I need to take supplements?
Not usually. A balanced, whole-food diet provides all the nutrients you need. Some patients on diuretics may lose magnesium or potassium, but supplements should only be taken if your doctor orders them. Don’t self-prescribe vitamins or minerals-they can interfere with your medications.
Next Steps
Start today. Write down everything you eat and drink for three days. Check the sodium on every label. Weigh yourself every morning. Talk to your doctor about seeing a dietitian. Make one small change this week-swap canned soup for homemade, skip the salt shaker, or choose fresh fruit instead of salty snacks.
You’re not just eating for today. You’re eating to live better tomorrow.


Jessica Engelhardt
November 18, 2025 AT 14:20So let me get this straight-you’re telling me I can’t have my daily bag of chips or a good old bowl of ramen anymore? My heart’s failing but my cravings are still 100% American? This is just another way for Big Pharma to sell more diuretics. I’ll stick to my salt and my sovereignty.
Lauren Hale
November 19, 2025 AT 13:11I’ve been managing HF for 7 years now. The sodium limit felt impossible at first-until I started cooking. No more frozen dinners. No more hidden salt in ‘healthy’ granola bars. I use smoked paprika, garlic powder, and lemon zest. My ankles don’t puff up anymore. It’s not about deprivation-it’s about retraining your palate. Your taste buds will thank you in 3 weeks. Seriously. Try it.
rachna jafri
November 21, 2025 AT 10:49They don’t want you to know this but sodium restriction is a corporate psyop. The FDA, Big Pharma, and the American Heart Association all profit from your fear. Real medicine is ancestral-salt is life. The body knows how to regulate. They just don’t want you eating real food from the earth. They want you dependent on pills and labeled ‘low-sodium’ sludge. Wake up. Your heart isn’t broken-it’s being poisoned by bureaucracy.
Hannah Machiorlete
November 21, 2025 AT 13:18ok so i tried the low sodium thing and honestly i felt like a zombie for 2 weeks. like no energy at all. then i went back to my normal diet and boom-i could breathe again. maybe my heart just hates being starved. who even knows anymore.
william volcoff
November 22, 2025 AT 06:26Interesting that they mention potassium-rich foods but don’t warn enough about the interaction with ACE inhibitors. I’ve seen patients crash from hyperkalemia because they ate 5 bananas a day thinking ‘it’s healthy.’ The real issue isn’t just sodium-it’s the blind spots in the guidelines. Always check labs. Always.
Mary Follero
November 23, 2025 AT 16:31One small change this week: swap the canned soup for a pot of homemade veggie broth with herbs. You’ll be shocked at how good it tastes. And you won’t feel like you’re on a punishment diet. Progress > perfection. You got this.
Arun Mohan
November 24, 2025 AT 21:39Let’s be honest-this whole low-sodium dogma is a middle-class luxury. People in developing nations don’t have access to fresh produce or organic quinoa. They eat what’s available. The real problem is systemic healthcare inequality, not someone’s choice to eat a bag of Doritos. Your ‘heart-healthy’ diet is a privilege, not a moral imperative.
Kenneth Meyer
November 25, 2025 AT 01:10There’s a deeper truth here: the body adapts. After 6 months of low sodium, I stopped craving salt entirely. Now, restaurant food tastes overwhelmingly gross. It’s not about willpower-it’s about rewiring your sensory expectations. The more you eat clean, the more processed food feels like a betrayal.
Donald Sanchez
November 25, 2025 AT 10:19bro i just use sea salt cause its 'natural' 😎 and i drink 3L of water a day bc why not 🤷♂️ also i take potassium pills from amazon lol
Greg Knight
November 26, 2025 AT 00:32I’ve coached 37 people with HF through dietary changes. The biggest hurdle? Not knowing where salt hides. I give them a cheat sheet: bread, soup, deli meat, sauces, frozen pizza, canned tuna, and even some breakfast cereals. Write it down. Stick it on the fridge. Then start swapping one thing a week. You don’t need to be perfect-you just need to be consistent. Small wins build momentum. You’re not alone in this.
darnell hunter
November 27, 2025 AT 18:39While the dietary recommendations presented are empirically supported, the absence of a formal meta-analysis citation for the 40% hospitalization reduction figure is methodologically problematic. Furthermore, the conflation of fluid restriction thresholds across heterogeneous patient subgroups lacks clinical granularity. A more rigorous approach would stratify recommendations by NYHA class and eGFR.