Bronchospasm therapy innovations: new options and what to ask your doctor
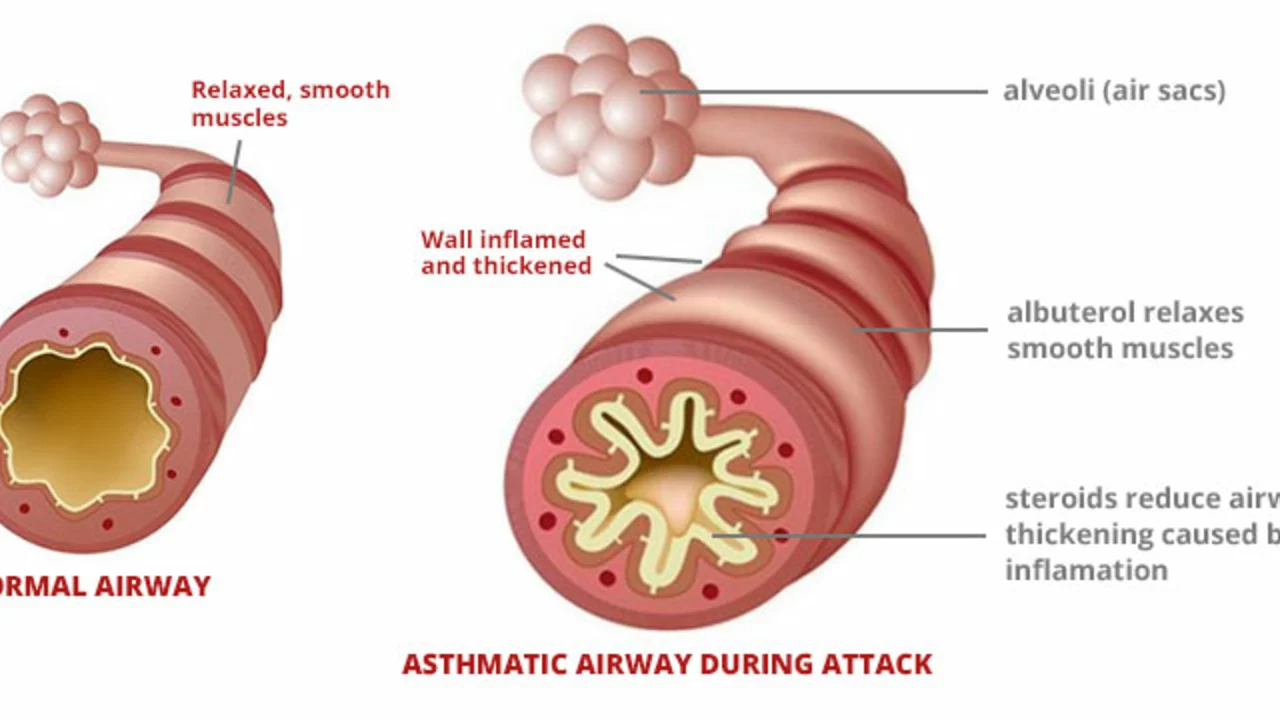
Bronchospasm means your airways tighten and you feel short of breath, wheeze, or cough. New treatments and devices aim to stop attacks faster and keep them away longer. This page focuses on practical, up-to-date options you can talk about with your care team.
Inhaler tech has moved fast. Smart inhalers track doses and remind you to use them. Breath‑actuated and soft‑mist inhalers deliver medicine more reliably when your breathing is weak. If you struggle with coordination, ask about these devices or using a spacer — they can make a big difference.
New drug combos give longer protection. Triple therapy inhalers and modern LABA/LAMA/ICS mixes reduce symptoms and flare-ups for many people with COPD and asthma. For some patients, newer inhaled formulations work better than older pairings because they control inflammation and open airways at the same time.
Biologic medicines are changing care for severe asthma. Drugs that block IgE or interleukins (IL‑5, IL‑4/13) cut the number and severity of bronchospasm episodes in people with specific biomarkers. Biologics require a prescription and regular follow up, but they can dramatically reduce steroid use and hospital visits for the right patient.
Bronchial thermoplasty remains an option for a subset of severe asthma patients. It uses controlled heat to reduce airway muscle and can lower attack frequency over time. The procedure is not for everyone, so discuss risks, benefits, and expected recovery with a specialist.
Device and delivery improvements
Nebulizers are smaller and faster than before. Mesh nebulizers give fine particles and work with many medicines, including combination treatments. Portable units mean you can treat a bad episode quickly when you’re out. Also, new rescue options pair a fast inhaled steroid with a fast bronchodilator for immediate symptom relief and inflammation control in one puff.
Practical tips for patients
Master your inhaler technique — it beats switching drugs if the device is wrong for you. Keep an action plan that tells you when to increase medicines and when to seek help. Track symptoms and triggers with your phone or a symptom diary. Ask your doctor about vaccine shots, comorbidity management, and avoiding triggers like smoke and strong odors.
Cost and access matter. New inhalers and biologics can be expensive. Ask about generics, patient assistance programs, or clinical trials. If you buy supplies online, verify the pharmacy’s credentials before you order.
Innovation in bronchospasm therapy is real, but not every new option fits every person. Bring questions, show your symptom diary, and ask for a demo of any device before you leave the clinic. That way you get a treatment plan that works in real life, not just on paper.
Want to learn more? Read articles comparing inhalers, guides on proper technique, and safety tips to verify pharmacies. We link to studies, practical how-tos, and cost-saving ideas so you can make smarter choices. If you're worried about symptoms, contact your doctor or local urgent care right away. Start timing your inhaler use with attacks.