Bronchospasm treatment: what to do now and how to prevent next time
Bronchospasm feels like your airways tightening — wheeze, chest tightness, and trouble breathing. You want quick relief and a plan so it doesn't happen again. Below are clear, practical steps for sudden attacks and real-world tips for long-term control.
Immediate steps for an attack
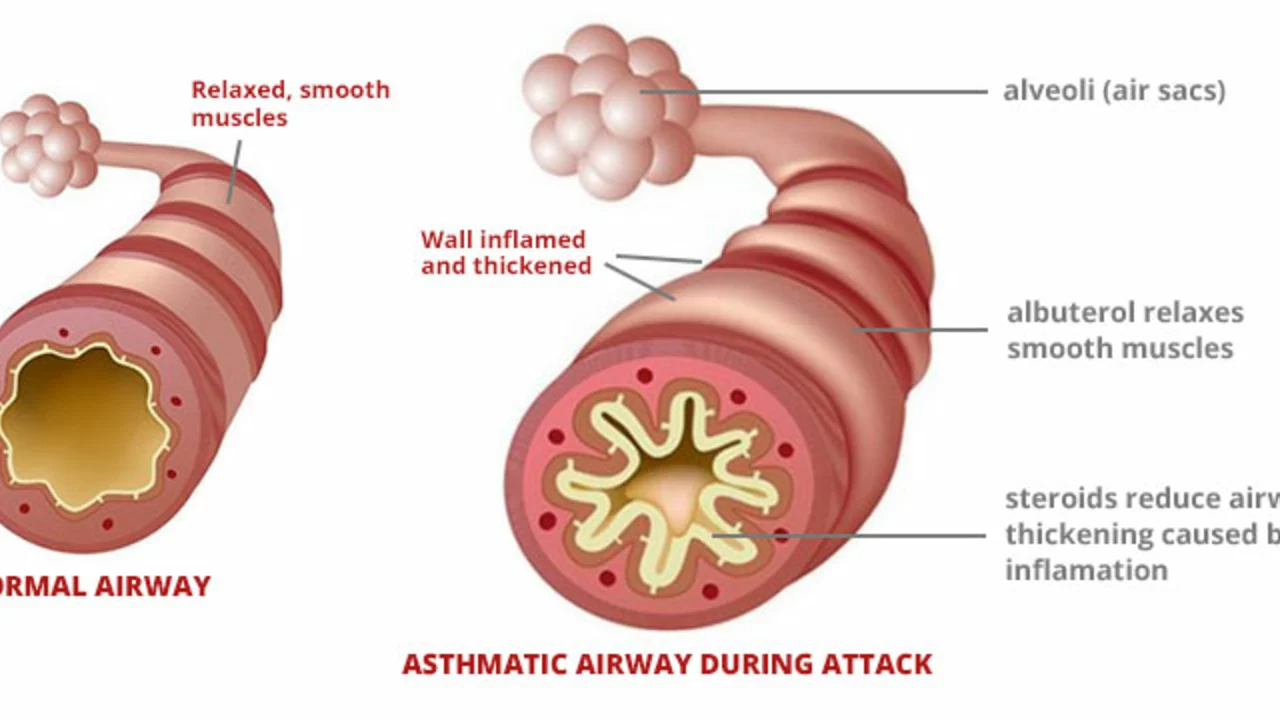
First, use your rescue inhaler. Short-acting beta-agonists (SABA) like albuterol work fast. Take 1–2 puffs, wait about a minute, then take another 1–2 puffs if needed. Use a spacer if you have one — it helps the medicine reach your lungs better.
If symptoms don’t improve after a few rounds with the inhaler, call emergency services. Signs you need urgent care include difficulty speaking, lips or face turning blue, fainting, or mental confusion. Emergency teams may give nebulized bronchodilators and oxygen and check your breathing more closely.
For some people, adding ipratropium (an inhaled anticholinergic) helps in the short term — this is common in emergency treatment or with a nebulizer. If your doctor prescribed a short oral steroid for flare-ups, start it as directed; it can stop the attack from getting worse over the next day or two.
Long-term control and prevention
Rescue inhalers are for sudden relief. To stop bronchospasm from coming back, you usually need daily controller therapy. For asthma that often means an inhaled corticosteroid (ICS) alone or combined with a long-acting bronchodilator (LABA). For COPD, long-acting bronchodilators (LABA or LAMA) are commonly used. Your doctor will match treatment to your symptoms and test results.
Learn proper inhaler technique — most people don’t use theirs correctly. Ask your clinician to watch you use it or bring your device to the visit. Spacers, mask attachments for kids, or switching device types can make a big difference.
Cut triggers. Common ones are smoke, cold air, respiratory infections, strong smells, exercise without a warm-up, and certain meds like oral beta-blockers. If allergies are a factor, allergy meds or immunotherapy might reduce bronchospasm episodes.
If you keep having attacks despite regular treatment, talk about advanced options: long-term macrolide antibiotics in selected COPD cases, biologic injections for severe allergic or eosinophilic asthma, or referral for pulmonary rehab. Also check for other problems that mimic bronchospasm, such as heart conditions or reflux disease.
Make an action plan with clear steps: which inhaler to use first, when to add steroids, when to call the doctor, and when to go to the ER. After any severe episode, schedule a follow-up within a few days so your provider can adjust meds and avoid repeat attacks.
Bronchospasm is treatable. Fast use of a rescue inhaler, knowing red flags, good inhaler technique, and a solid prevention plan together keep you breathing easier and more confident.