Diverticulitis: what to watch for and what to do
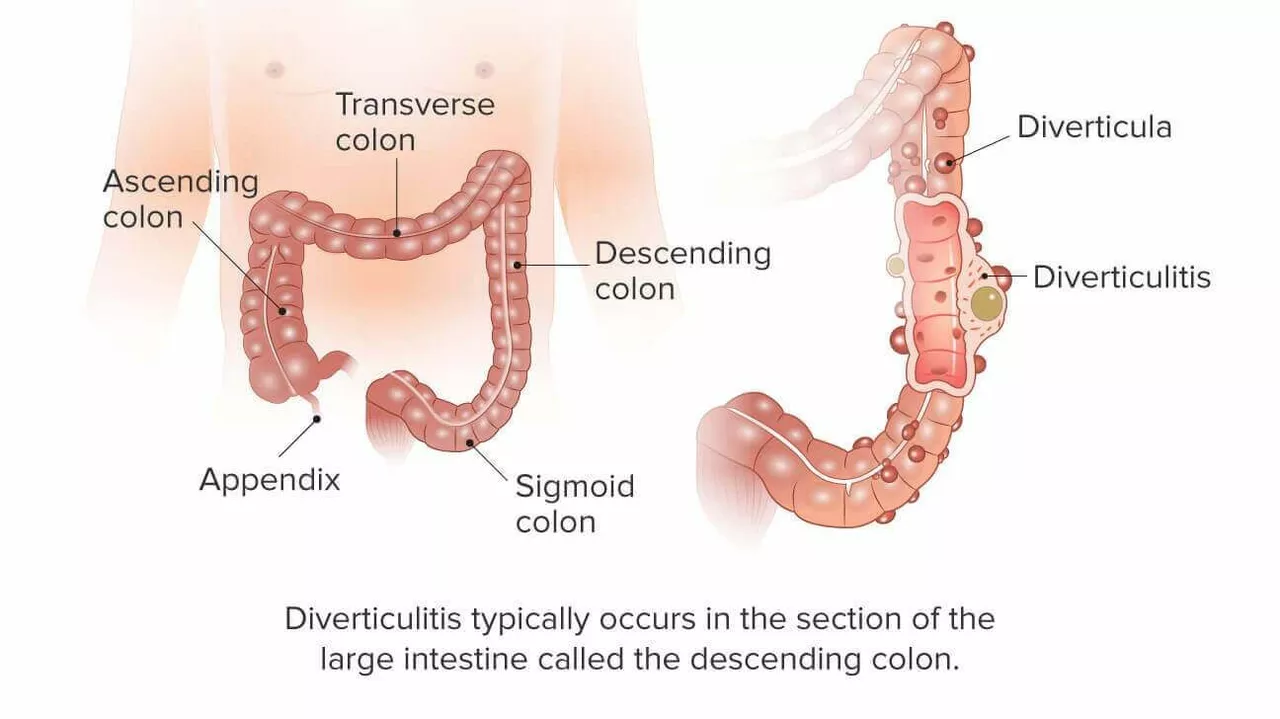
Sudden lower belly pain—often on the left side—plus fever and a change in bowel habits? That can be diverticulitis: inflammation or infection of small pouches (diverticula) in the colon. It sounds scary, but most people get clear care and recover well when they act early.
How do you tell if it’s diverticulitis? Look for steady, localized pain (not just cramping), fever, nausea, and constipation or diarrhea. Your doctor will usually confirm with a CT scan. That test tells them if it’s a simple flare or something more serious like an abscess or perforation.
Treatment you can expect
Mild cases are often treated at home. That can mean rest, pain relief (acetaminophen is usually preferred), clear liquids for a short time, then a gradual return to low-residue foods. Doctors sometimes prescribe antibiotics, though current practice varies for mild episodes—your clinician will decide based on your symptoms and scan results.
If the CT shows a complication (abscess, perforation, fistula or bowel blockage), you may need IV antibiotics, drainage of an abscess, or surgery. Emergency signs to watch for: high fever, worsening or spreading belly pain, vomiting, fainting, or a hard, tender belly. If any of those happen, go to the ER right away.
Diet, recovery, and prevention
During a flare some people do better on clear liquids for 24–48 hours, then slowly add low-fiber foods. Once healed, switch to a high-fiber diet to help prevent future attacks—aim for about 25–30 grams of fiber a day from fruits, vegetables, whole grains, and legumes. Also drink plenty of water and stay active; walking 30 minutes most days helps bowel regularity.
Avoidance tips that actually help: quit smoking, maintain a healthy weight, and don’t overuse NSAIDs (they can raise complication risk). Stool softeners or gentle fiber supplements can be useful if you tend to be constipated, but don’t use strong laxatives during an active infection unless your doctor says it’s OK.
After a first confirmed episode, your doctor will usually recommend a follow-up colonoscopy in about 6–8 weeks once inflammation has settled. This checks for other problems like polyps or cancer that can mimic diverticulitis.
Bottom line: most diverticulitis cases get better with timely care and lifestyle changes. Keep an eye on symptoms, call your doctor early, and seek emergency care for severe signs. Want help making a simple high-fiber meal plan or questions to ask your doctor? I can help with practical tips you can use right away.