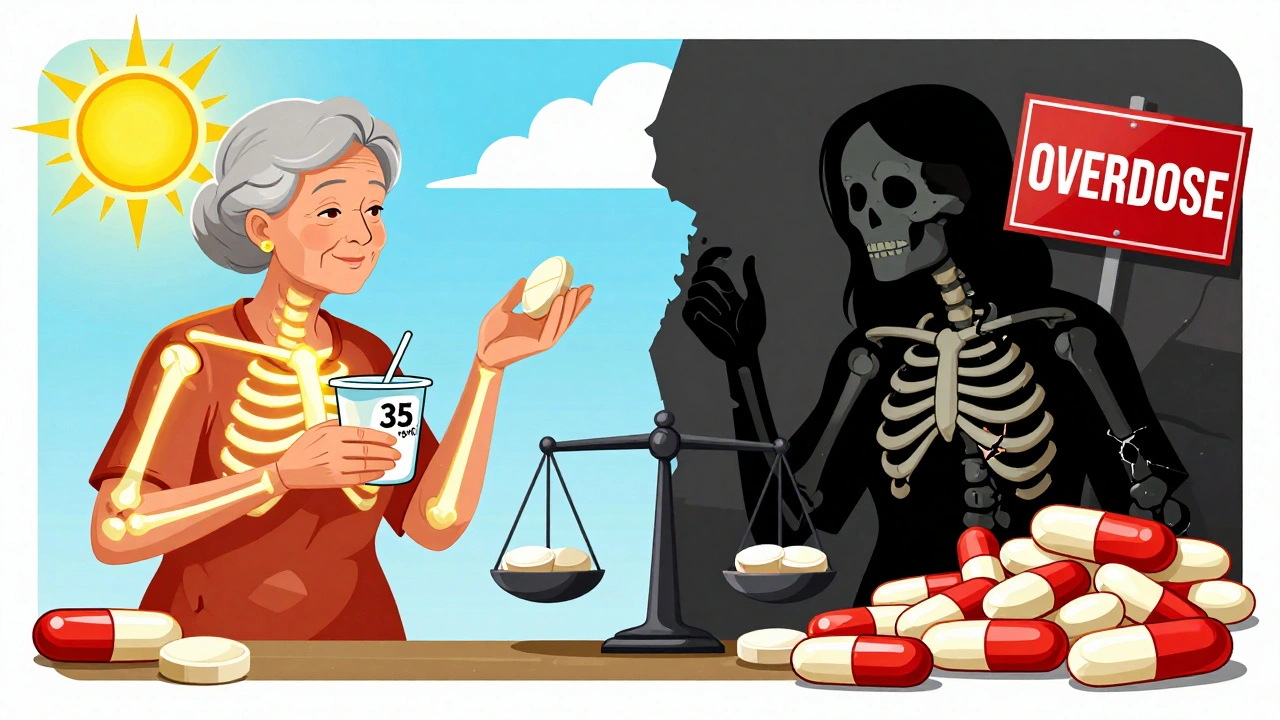
For decades, doctors told us: take vitamin D to keep your bones strong. It’s simple, logical, and seemed backed by science. But today, the story is far more complicated. High-dose vitamin D supplements aren’t helping most people avoid fractures - and in some cases, they might actually be hurting bone density. If you’re wondering whether you should be popping vitamin D pills, what dose is right, or if your bone scan results should worry you, you’re not alone. The truth isn’t in a single recommendation. It’s in your baseline level, your age, your body weight, and even what you ate for breakfast.
Why Vitamin D Matters for Bones - and Why It’s Not Always the Answer
Vitamin D doesn’t build bone directly. It’s the gatekeeper for calcium. Without enough vitamin D, your body absorbs just 10-15% of the calcium you eat. With enough, that jumps to 60-80%. That’s why rickets - the childhood disease that causes soft, bent bones - disappeared after vitamin D was added to milk in the 1930s. Today, the same mechanism keeps adult bones from crumbling. Vitamin D also helps your muscles stay strong, which reduces the chance of falls that lead to fractures.
But here’s the twist: most healthy adults already get enough vitamin D from food and sun. A 2022 Harvard study tracking over 25,000 people found that taking 2,000 IU daily for five years didn’t lower fracture rates at all. Not in men over 50. Not in women over 55. Not even in those with low baseline levels. If your vitamin D level is above 20 ng/mL, extra pills likely won’t help your bones.
What’s a "Normal" Vitamin D Level? The Numbers That Matter
Doctors often test your serum 25-hydroxyvitamin D - the main form measured in blood. The Endocrine Society says you need at least 30 ng/mL for optimal bone health. But that number is being questioned. The VITAL trial, one of the largest studies ever done on vitamin D, found no benefit from aiming for 30 ng/mL in healthy older adults. In fact, some evidence suggests that levels above 40 ng/mL might not add any extra protection.
Here’s what the data actually shows:
- Below 20 ng/mL (50 nmol/L): Deficient. You’re at higher risk for bone loss and fractures.
- 21-29 ng/mL (52.5-72.5 nmol/L): Insufficient. You may benefit from modest supplementation.
- 30-40 ng/mL (75-100 nmol/L): Sufficient. No added benefit from going higher.
- Above 50 ng/mL (125 nmol/L): Potential risk. Higher levels linked to lower bone density in some studies.
That’s why testing before supplementing matters. Taking 5,000 IU a day when you’re already at 35 ng/mL isn’t helping - it might be doing damage.
The Dose That Hurts: Why More Isn’t Better
In 2020, a major JAMA study shocked the medical world. Participants who took 4,000 IU or 10,000 IU of vitamin D daily for three years ended up with lower bone density than those taking 400 IU. The higher the dose, the worse the result. At 10,000 IU, tibial bone density dropped significantly. This wasn’t a fluke. It matched findings from other trials showing that excessive vitamin D can trigger bone breakdown.
Why? Too much vitamin D may overstimulate cells that break down bone (osteoclasts). It can also raise blood calcium levels, which your body then tries to remove by pulling calcium out of bone. This isn’t theoretical - it’s measurable. One Reddit user reported a 3.7% drop in femoral neck density after two years of 10,000 IU daily. Another saw a 2.1% gain after increasing from 1,000 to 5,000 IU. The difference? Baseline levels. The first was likely already sufficient. The second was deficient.
Who Actually Benefits From Supplements?
Not everyone. But some people do. If you fall into one of these groups, supplements can make a real difference:
- People with diagnosed deficiency: Below 20 ng/mL. A short course of 50,000 IU weekly for 6-8 weeks followed by 800-1,000 IU daily is standard.
- Older adults with low sun exposure: Especially those who live in northern latitudes, wear full clothing outdoors, or stay indoors most days.
- People with obesity (BMI ≥30): Fat cells trap vitamin D. You may need double the dose to reach the same blood level as someone with normal weight.
- Those with osteoporosis or high fracture risk: The International Osteoporosis Foundation recommends supplementation as part of a broader treatment plan - but always paired with calcium and other bone meds if prescribed.
For everyone else? Focus on food and sun. Salmon (570 IU per 3 oz), fortified milk (100 IU per cup), eggs (44 IU per yolk), and mushrooms exposed to UV light are your best bets. Ten to 15 minutes of midday sun on arms and legs two to three times a week can produce 10,000-20,000 IU of vitamin D - naturally, safely, and without pills.
Calcium + Vitamin D: The Only Combo That Works for Fractures
Here’s the most important takeaway: vitamin D alone rarely prevents fractures. But when paired with calcium, it does.
A 2023 meta-analysis of 11 studies found that taking both reduced total fracture risk by 15% and hip fracture risk by 30%. But here’s the catch: the benefit vanished if vitamin D doses went above 400 IU per day. In fact, higher doses showed no improvement in femoral neck bone density. That means: if you’re taking vitamin D to protect your hips, keep it at 800 IU or less - and make sure you’re getting 1,000-1,200 mg of calcium daily from food or supplements.
Too much calcium without enough vitamin D? It can build up in arteries. Too much vitamin D without enough calcium? Your body pulls calcium from your bones to balance blood levels. The two work together. Neither works well alone.

Supplement Quality and Timing: What No One Tells You
Not all vitamin D pills are created equal. ConsumerLab tested 30 brands in 2022. Fifteen percent contained less than 90% of the labeled dose. One brand had only 72% of what was printed on the bottle. Another exceeded its label by 28%. If you’re paying for 5,000 IU, you might be getting 3,600 - or 6,400. That’s a big difference when you’re trying to hit a precise target.
Choose brands with USP or NSF certification. These are third-party tested for accuracy. Avoid ultra-cheap generics unless they’re certified.
And timing matters. Take your vitamin D with your biggest meal - preferably dinner. A 2015 study found absorption jumped 56.7% when taken with food compared to fasting. Fat helps dissolve it. A glass of milk, a spoonful of yogurt, or a handful of nuts with your pill makes a measurable difference.
What to Do Now: A Simple Action Plan
Don’t guess. Don’t follow trends. Don’t take 10,000 IU because someone on Reddit said it helped. Do this instead:
- Get tested. Ask your doctor for a 25(OH)D blood test. Don’t skip this step.
- If your level is below 20 ng/mL: Follow your doctor’s protocol - likely a short high-dose course, then 800-1,000 IU daily.
- If it’s 21-29 ng/mL: Take 1,000 IU daily. Re-test in 3 months.
- If it’s 30-40 ng/mL: No supplement needed. Get sun, eat fatty fish, and focus on calcium.
- If it’s above 40 ng/mL: Stop or reduce supplements. You may be harming your bones.
And if you’re over 60, make sure you’re getting 1,000-1,200 mg of calcium daily - from yogurt, cheese, leafy greens, or a supplement if needed. Pair it with 800 IU of vitamin D. That’s the only combo proven to cut fracture risk.
What’s Next? The Science Is Still Evolving
The D-Health Trial in Australia, finishing in 2024, is testing monthly doses of 60,000 IU - far higher than daily pills. Early results suggest monthly dosing may be safer than daily megadoses. Meanwhile, new drugs like eldecalcitol (used in Japan) are showing promise for osteoporosis treatment, with 37% fewer spine fractures than standard vitamin D.
But for now, the message is clear: vitamin D is not a magic bone pill. It’s a nutrient. Like iron or vitamin B12, you need the right amount - not more. Too little causes harm. Too much can too. The goal isn’t to max out your blood level. It’s to stay in the sweet spot - and let your bones do the rest.
How do I know if I’m deficient in vitamin D?
The only reliable way is a blood test for 25-hydroxyvitamin D. Symptoms like fatigue, muscle weakness, or bone pain are vague and often mistaken for other issues. Don’t assume you’re deficient just because you don’t get much sun. Many people with low sun exposure still have normal levels. Testing is the only way to be sure.
Can I get enough vitamin D from food alone?
It’s very hard. Even a 3-ounce serving of salmon gives you 570 IU - less than half the daily amount many experts recommend for at-risk groups. Fortified milk adds 100 IU per cup. You’d need to eat 6-8 cups of milk daily to hit 1,000 IU. Most people need some supplementation - but only if their blood level is low.
Is vitamin D3 better than D2?
Yes. Vitamin D3 (cholecalciferol), from animal sources or sunlight, raises blood levels about 87% more effectively than D2 (ergocalciferol), which comes from plants. Most supplements and prescriptions use D3. Stick with it unless you’re vegan and your doctor approves D2.
Should I take vitamin D with calcium?
Only if your blood level is low and you’re at risk for fractures. For most healthy adults, getting calcium from food (dairy, greens, tofu) is better than supplements. If you do take calcium pills, choose ones with vitamin D already added - and keep the vitamin D dose under 800 IU. Higher doses cancel out the benefit.
Can too much vitamin D cause kidney stones?
It’s possible, but rare. Very high doses (above 10,000 IU daily for months) can raise blood calcium levels, which may increase stone risk in people prone to them. For most people, even 4,000 IU daily is safe. The bigger risk isn’t kidney stones - it’s losing bone density. That’s what the research shows.


Courtney Black
December 10, 2025 AT 09:03So let me get this straight - we’ve been sold a myth for decades, and now the science says: stop taking the pills unless you’re actually deficient? I’m not mad, I’m just disappointed in my entire generation’s relationship with supplements.
We treat vitamins like candy. Buy the biggest bottle. Take it with breakfast. Hope for magic. Meanwhile, the real fix - sun, food, movement - is free and has been staring us in the face since the 1930s.
It’s not about vitamin D. It’s about how we’ve outsourced our health to pills and algorithms.
iswarya bala
December 10, 2025 AT 21:23omg this is so true!! i was takin 5000iu daily for 2 years n my doc finally said u r fine stop!! my level was 38 n i felt worse 😅 now i just walk outside n eat yogurt n feel way better!! thx for the clarity!!
Simran Chettiar
December 11, 2025 AT 10:21It is an incontrovertible fact, grounded in empirical observation and longitudinal clinical data, that the medical establishment has, for the better part of the last century, conflated correlation with causation in the domain of nutritional supplementation.
The paradigm shift now underway - wherein vitamin D is no longer viewed as a panacea but as a context-dependent nutrient - reflects a broader epistemological correction in public health discourse.
One cannot simply extrapolate biochemical mechanisms into population-wide prescriptions without accounting for individual homeostatic variance, dietary intake, and environmental exposure.
The notion that more is better is not merely flawed - it is a relic of pharmaceutical marketing masquerading as preventive medicine.
And yet, the cultural addiction to supplementation persists, not because of science, but because of the psychological comfort derived from the ritual of ingestion.
Philippa Barraclough
December 12, 2025 AT 17:02Interesting that the JAMA study showed bone density loss at 4,000 and 10,000 IU. I wonder if the participants were also taking calcium supplements or not. That’s a critical variable - vitamin D without adequate calcium could theoretically trigger bone resorption as the body tries to maintain serum calcium levels.
Also, the timing of supplementation relative to meals matters, as the post notes. Absorption is significantly higher with fat intake. I’ve seen studies where fasting vitamin D intake resulted in less than 30% bioavailability.
And the brand variability is terrifying. If you’re paying $20 for a bottle labeled 5,000 IU but only getting 3,600, you’re not just wasting money - you’re potentially missing your target without realizing it.
It’s not just about the dose. It’s about consistency, quality, and context. Most people treat it like a one-size-fits-all solution. It’s not.
Olivia Portier
December 13, 2025 AT 09:09Y’all need to stop panicking and start testing!!
If your level is 32? Chill. Eat your cheese. Walk in the sun. Stop buying those giant bottles.
If it’s 18? Do the 50k weekly for 8 weeks. Then go to 1000 IU. You’ll feel like a new person.
And if you’re over 60? Calcium + 800 IU D. That’s it. No magic. No hype. Just science.
You got this. You don’t need to be perfect. You just need to be informed. 💪
Brianna Black
December 14, 2025 AT 09:51Let me be the first to say this: the entire vitamin D industry is a beautifully packaged placebo. We live in a culture that equates health with consumption. If you don’t take something, you’re not trying. If you don’t take enough, you’re failing.
Meanwhile, the Inuit, who consume massive amounts of fatty fish and have minimal sun exposure, maintain bone densities that outperform most Western populations on supplements.
It’s not the vitamin D. It’s the lifestyle.
We’ve been sold a lie wrapped in a lab coat.
And now we’re paying for it - in pills, in blood tests, in anxiety.
Go outside. Eat real food. Sleep. Move.
That’s the real supplement.
Shubham Mathur
December 14, 2025 AT 13:05People keep saying 'test first' like it's hard but you just ask your doctor and they do it for free under Medicare in the US and most places
My uncle took 10k IU for 3 years and lost 5% bone density then stopped and it bounced back
So stop being lazy and get tested
Also D3 not D2
And take it with dinner not breakfast
And stop buying random brands
USP certified or don't bother
And if you're not deficient you're just wasting money and risking your bones
That's it
Ruth Witte
December 14, 2025 AT 14:01OMG I JUST STOPPED MY 5000IU AND NOW I’M EATING SALMON 3X A WEEK AND I CAN FEEL MY LEGS WORKING AGAIN 😭🔥
Also I walk barefoot in the backyard at noon. It’s like nature’s vitamin D machine 🌞💖
Who knew the answer was outside and not in a bottle??
Lauren Dare
December 15, 2025 AT 12:59Of course the FDA doesn’t regulate supplement dosing. Of course brands lie on labels. Of course people think ‘natural’ means ‘safe in any quantity.’
It’s not ignorance. It’s willful suspension of critical thinking wrapped in wellness branding.
And yet, we’re shocked when science contradicts the Instagram influencer who took 20,000 IU and ‘feels amazing.’
Let me guess - she also drinks lemon water every morning and does cold plunges.
Reality has no algorithm.
Andrea DeWinter
December 16, 2025 AT 00:19For anyone over 60, especially if you’ve had a fracture or are on steroids - calcium and vitamin D together are non-negotiable. But here’s the thing: most people get calcium from dairy and greens and don’t need a pill. If you’re vegan or lactose intolerant, then yes - supplement, but pair it with D under 800 IU.
Also, if you’re obese, you need more - but not because you’re broken. Because fat absorbs vitamin D like a sponge. Your body isn’t defective. It’s just biology.
Test. Don’t guess. And don’t shame people for taking what they need. This isn’t a moral issue. It’s a physiological one.
precious amzy
December 16, 2025 AT 12:21One cannot help but observe the troubling epistemological regression inherent in the contemporary discourse surrounding nutritional supplementation. The conflation of statistical association with causal efficacy - a fallacy that has plagued epidemiology since its inception - is now institutionalized as public health doctrine.
The VITAL trial, while methodologically rigorous, remains subject to the confounding variable of dietary calcium intake, which was neither standardized nor stratified in its cohort analysis.
Moreover, the arbitrary delineation of serum 25(OH)D thresholds - 20, 30, 40 ng/mL - is a construct of consensus, not biological imperative. The human organism does not recognize decimal points.
And yet, we have elevated these arbitrary cutoffs to dogma, prescribing interventions based not on individual physiology, but on population medians.
It is not vitamin D that is the problem.
It is the reductionist impulse to quantify human health in nanograms per milliliter.