Electronic prescribing was supposed to fix medication mistakes. It cut down on illegible handwriting, reduced dosage confusion, and made refills easier. But in the real world, it didn’t erase errors - it just changed them. Now, instead of doctors scribbling "take 1 tablet three times a day" in messy handwriting, pharmacists are staring at screens wondering why a prescription says "1 TAB PO DAILY" and the system reads it as "10 TAB PO DAILY." This isn’t a glitch. It’s a systemic flaw. And it’s happening every day in pharmacies across the U.S. and Australia.
Why E-Prescribing Still Causes Errors
The promise of e-prescribing was simple: digitize the prescription, remove human error, and make everything safer. And it worked - sort of. A 2008 study in JAMIA found that e-prescribing cut overall prescribing errors by as much as 99% in some settings. But here’s the catch: the errors that remained? They were mostly transcription errors. These aren’t mistakes made by doctors. They happen when data moves between systems - from an EHR to a pharmacy’s system, from one vendor’s software to another. The prescription gets sent, but the format changes. The meaning gets lost. Take this real example from a pharmacy technician in Melbourne: A patient’s prescription says, "Take 1 tablet by mouth daily." The EHR sends it as "1 TAB PO DAILY." The pharmacy’s system, built on older standards, misreads "DAILY" as "10 DAILY" because of how the code is parsed. The patient ends up with a 10-fold overdose. That’s not a typo. That’s a system failure. The problem isn’t one system. It’s the patchwork of 50+ different e-prescribing platforms that don’t talk to each other. Epic, Cerner, DrFirst, QS/1, Pioneer - each has its own way of labeling dosing instructions. And when a prescription moves from a hospital using Epic to a community pharmacy using QS/1, the sig (signa) often breaks. A 2022 Surescripts report found that 41% of pharmacists spend 15 to 30 minutes a day just fixing these broken prescriptions. That’s not efficiency. That’s damage control.The Six Evidence-Based Fixes
The Agency for Healthcare Research and Quality (AHRQ) studied this problem for years. In 2021, they published a report that didn’t just identify the issue - it gave clear, tested solutions. Six strategies cut transcription errors by more than half. Here’s what actually works:- Standardized sig formatting - Instead of letting doctors type "take one pill every morning," the system forces them to pick from a dropdown: "1 tablet orally once daily." This simple change reduced errors by 41% in pilot clinics.
- CancelRx protocol - When a doctor changes a prescription, they used to send a new one. The old one stayed in the system. Pharmacists had to guess which one was active. CancelRx lets providers electronically cancel old prescriptions. This cut confusion errors by 63%.
- Single shared medication list - If a patient has 12 medications, and each one comes from a different system, reconciliation becomes a nightmare. A unified, real-time list that updates across all providers and pharmacies cuts reconciliation errors by 52%.
- Structured indication entry - When a doctor writes "for pain," the system doesn’t know if it’s arthritis, back pain, or neuropathy. But if they select "chronic low back pain" from a menu, the pharmacy system can flag dangerous interactions. This reduced indication-drug mismatches by 79%.
- Pharmacy-prescriber connectivity - When EHRs and pharmacy systems speak the same language - using HL7 FHIR Release 4.0.1 - manual re-entry drops by 92%. That’s not a guess. That’s what happened in an ISMP Canada case study.
- Redesigned workflow for modifications - If a doctor needs to change a prescription after it’s sent, they shouldn’t have to call the pharmacy. Systems that allow real-time edits - not just cancellations - cut confusion errors by 67%.
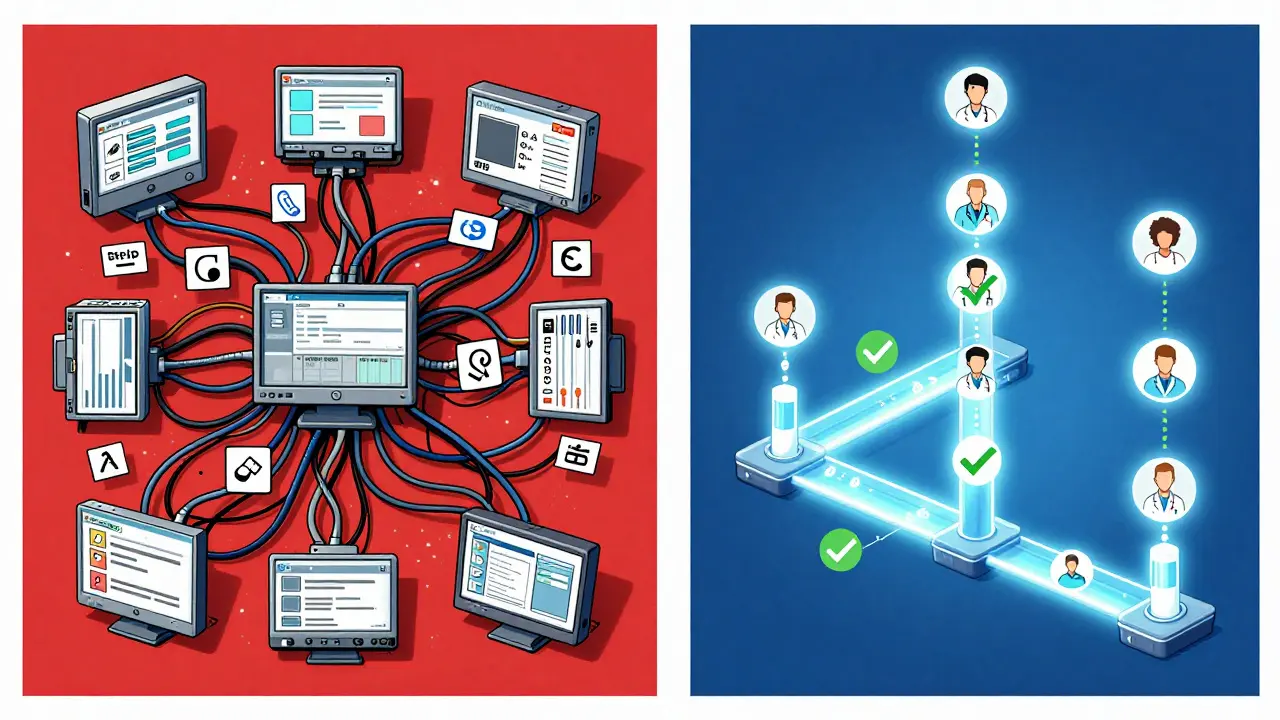
Integrated Systems Beat Standalone
Not all e-prescribing systems are equal. There’s a big difference between a standalone e-prescribing tool and one built into the full electronic health record (EHR). A 2019 KLAS report found that standalone systems like DrFirst Rcopia had 42% fewer transcription errors than EHR-integrated ones. At first, that sounds backward. But here’s why: standalone tools are designed for one thing - sending prescriptions. They don’t try to do everything. They’re lean. Focused. Clean. But here’s the twist: when those standalone tools are connected to a full EHR, errors drop even further. The real win comes from integration - not just e-prescribing, but full EHR-pharmacy integration. A 2021 JAMIA study showed that Epic’s Hyperspace system reduced overall prescribing errors by 84% because it linked prescribing, patient history, allergies, and pharmacy data in one place. The difference? A single shared medication list. When a patient’s list updates in real time across the hospital, the clinic, and the pharmacy, no one has to guess. No one has to retype. No one has to call back. In fact, a 2022 MGMA case study found that practices using Epic integrated with CVS pharmacies had 92% fewer transcription errors. Why? Because the system didn’t just send a prescription - it sent the full context: allergies, past reactions, current meds, and the reason for the drug.What’s Broken Today
Despite all the progress, the system still fails in predictable ways:- Legacy systems - 63% of providers say their old software can’t talk to new ones. This is especially common in small practices.
- Alert fatigue - Doctors get so many warnings they start clicking past them. Dr. Joan Ash found that 34% of transcription errors happen because providers override safety alerts without reading them.
- Missing indications - If a doctor prescribes methotrexate for rheumatoid arthritis but doesn’t say so, the pharmacy can’t know if it’s safe to give with other drugs. Dr. David Bates says adding indications could eliminate 78% of dosing frequency errors.
- Controlled substance rules - Even though the DEA now requires e-prescribing for Schedule II drugs (like oxycodone), some systems still allow faxed copies. That’s a loophole. And it’s a source of error.

What’s Changing - Fast
The rules are shifting. And so are the tools. In 2023, the ONC released its Interoperability Roadmap. By 2025, all e-prescribing systems must use API-based connections - no more faxing, no more manual entry. This isn’t a suggestion. It’s a requirement. And the government is funding it: $15 million is going to small practices to upgrade their systems. The real game-changer? HL7 FHIR. This isn’t just another standard. It’s the language all systems will speak. In 2023, the Da Vinci Project tested FHIR-based prescription exchange. Result? 98% fewer errors. That’s not a typo. That’s a revolution. And AI is coming. Epic’s DoseMeRx, in pilot phase since 2023, uses machine learning to predict when a prescription might be wrong - not just based on dosage, but on patient history, lab results, and even weather patterns (yes, cold weather affects how some drugs are metabolized). Early results show a 65% drop in transcription errors. By 2026, this could be standard.What You Can Do Right Now
You don’t have to wait for a $10 million EHR upgrade to fix this. Here’s what any practice or pharmacy can do today:- Switch to structured sigs - If your system lets you pick from dropdowns instead of typing, use them. Always.
- Enable CancelRx - If your EHR supports it, turn it on. It takes 10 minutes.
- Check the sig before sending - Don’t just click "Send." Look at the text. Does it say "1 TAB PO DAILY"? That’s a red flag. Change it to "1 tablet by mouth once daily."
- Ask for FHIR - If your pharmacy or EHR vendor says they’re "interoperable," ask: "Do you use HL7 FHIR Release 4.0.1?" If they don’t know, they’re not ready.
- Train your staff - Pharmacists need 3.2 hours of training to handle new error patterns. Prescribers need 4.7 hours. Don’t skip it.
Transcription errors aren’t inevitable. They’re engineered. And they can be fixed - not with more technology, but with better design. Better standards. Better communication. The tools are here. The data is clear. What’s missing is the will to use them right.
What’s the most common transcription error in e-prescribing?
The most common error is misinterpretation of dosing instructions. For example, when a prescription says "1 TAB PO DAILY," some pharmacy systems read "DAILY" as "10 DAILY," leading to a 10-fold overdose. This happens because older systems use abbreviations like "TAB" and "PO" inconsistently, and don’t recognize standard clinical language. Structured sigs - where doctors pick from predefined options - reduce this error by 41%.
Do all e-prescribing systems have the same error rates?
No. Standalone systems like DrFirst Rcopia have fewer transcription errors than EHR-integrated ones - 42% fewer, according to a 2019 KLAS report. But when an EHR is fully integrated with pharmacy systems (like Epic + CVS), transcription errors drop by 55% more than standalone systems. The key isn’t the type of system - it’s whether it connects directly to the pharmacy’s system using modern standards like FHIR.
Can pharmacists fix these errors themselves?
They can, but they shouldn’t have to. Right now, 41% of pharmacists spend 15-30 minutes daily clarifying e-prescription errors. That’s not safe. It’s unsustainable. The goal isn’t to train pharmacists to be error detectives - it’s to stop the errors from happening in the first place. The fix is upstream: better systems, standardized formats, and direct connectivity.
Why do some doctors still write prescriptions by hand?
Some still do because their EHR system is clunky, slow, or doesn’t support e-prescribing well. Others work in settings where the pharmacy system can’t receive electronic prescriptions - like rural clinics with outdated tech. But under Medicare Part D rules, e-prescribing is required. Faxed or handwritten prescriptions for controlled substances are no longer allowed after 2021. The trend is clear: handwritten scripts are becoming illegal, not just outdated.
Is FHIR the solution to all e-prescribing errors?
FHIR (Fast Healthcare Interoperability Resources) is the most promising standard we have. It allows systems to exchange data in a consistent, machine-readable way. In pilot studies, FHIR reduced transcription errors by 98%. But it’s not magic. It only works if every system - from the doctor’s EHR to the pharmacy’s software - adopts it. Until then, errors will persist. The ONC mandates FHIR adoption by 2025, so full implementation is coming. But until then, practices should demand FHIR compliance from their vendors.
How can small practices afford to fix these errors?
The U.S. government is helping. In 2023, the ONC allocated $15 million to support small practices (<10 providers) in upgrading to FHIR-compliant e-prescribing systems. Many vendors now offer low-cost or subscription-based models. Surescripts’ Pharmacy Health Information Exchange, launched in 2020, reduced transcription errors by 88% in pilot sites - and it’s free for many small practices. The cost of not fixing it - patient harm, lawsuits, regulatory penalties - is far higher.



Robert Petersen
February 14, 2026 AT 15:34Love this breakdown. Seriously, we’ve all seen that "1 TAB PO DAILY" turn into "10 TAB" and watched pharmacists panic. It’s wild how something so simple breaks so hard. The fix isn’t fancy tech-it’s just forcing dropdowns. Why are we still letting people type? 🤦♂️
Craig Staszak
February 15, 2026 AT 23:49Been in pharmacy for 15 years and this is the #1 headache. No one talks about how the sigs get butchered during handoffs. I’ve seen "qhs" turned into "10 hs" because some system thought it was a number. We’re not fixing the problem-we’re just training staff to be human spellcheckers
alex clo
February 17, 2026 AT 23:22While the proposed solutions are empirically sound, it is imperative to recognize that systemic interoperability requires not only technological alignment but also institutional governance. The adoption of HL7 FHIR Release 4.0.1 is not merely a technical upgrade-it represents a paradigm shift in clinical data exchange that necessitates regulatory alignment, vendor accountability, and workflow redesign at the organizational level.
Alyssa Williams
February 18, 2026 AT 15:34OMG YES. I work in a small clinic and we just turned on structured sigs last month. Our med errors dropped like a rock. No more "take 1 or 2"-now it’s "1 tablet once daily" or "2 tablets once daily". Simple. Clear. No guesswork. Why didn’t we do this sooner??
Ernie Simsek
February 20, 2026 AT 15:29LMAO at "10 TAB PO DAILY" 😂. I swear half the time I think the systems are trolling us. Like come on, who designed this? Also, FHIR is literally the hero we didn’t know we needed. 🚀🔥 If your vendor says "we’re interoperable" but doesn’t mention FHIR, run. Run far away. 🏃♂️💨
Joanne Tan
February 22, 2026 AT 08:45My boss just told me to "just call the prescriber" when a sig breaks. Like… we’re doing 15 of these a day. I’m not a phone operator. We need CancelRx turned on. It’s literally one click. Why is this still not standard??
Stacie Willhite
February 23, 2026 AT 15:08Reading this made me realize how much silent stress pharmacists carry. We’re not just filling scripts-we’re decoding broken messages from systems that don’t talk to each other. I wish more people knew how much of our day is spent untangling this. It’s not just busywork. It’s patient safety.
Gabriella Adams
February 24, 2026 AT 06:32There’s a quiet revolution happening in e-prescribing that nobody’s talking about: the shift from "fixing errors after they happen" to "preventing them at the source." The six strategies outlined here aren’t just best practices-they’re baseline requirements for modern care. FHIR isn’t a feature. It’s the foundation. And until every vendor adopts it uniformly, we’re all just dancing on broken code.
Robert Petersen
February 24, 2026 AT 13:13^^^ This. And honestly? The fact that we still have to manually check "DAILY" vs "10 DAILY" in 2025 is embarrassing. We’re not fixing tech-we’re fixing laziness. If the system can’t handle "once daily" without turning it into "10 daily," it’s not broken. It’s negligent.