Diuretics: What They Do and How to Use Them Safely
Diuretics can drop your weight on the scale fast — but that's not the same as fat loss. They push water and salt out through your kidneys, and that can help if fluid is building up in your body. Used the right way, diuretics treat high blood pressure, swelling from heart or liver problems, and certain kidney issues. Used the wrong way, they cause dizzy spells, low potassium, and trouble with kidneys.
How diuretics work and main types
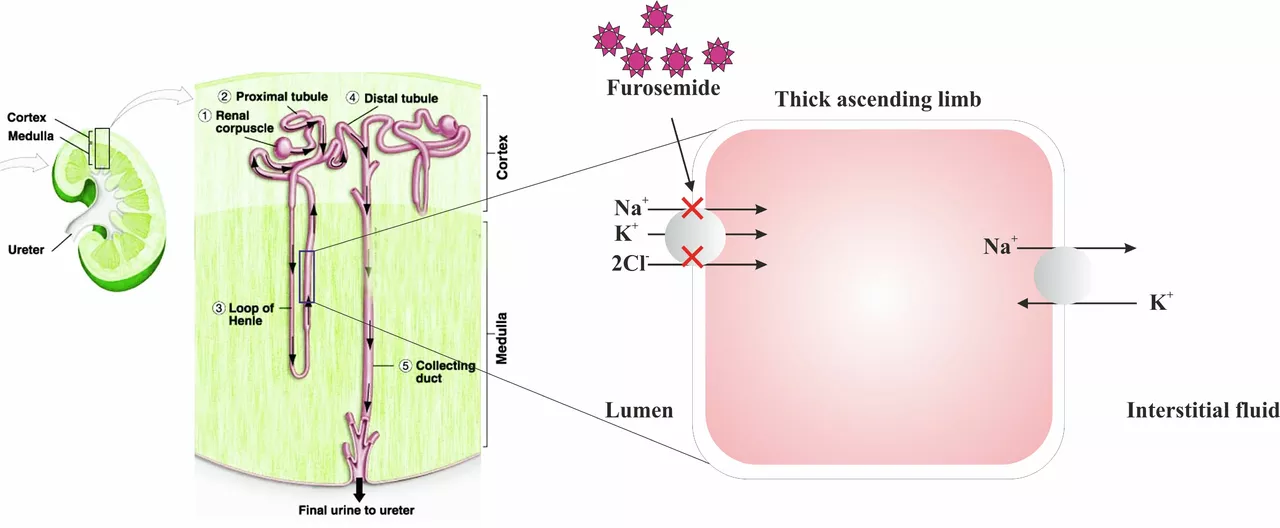
There are three common types people hear about. Thiazide diuretics (like hydrochlorothiazide) are often first choice for mild high blood pressure. Loop diuretics (like furosemide) are stronger and used with heart failure or big fluid overload. Potassium‑sparing diuretics (like spironolactone) keep potassium from dropping but are weaker at removing fluid. Each type works in a different part of the kidney and affects how much sodium and water are lost.
Diuretics are prescription medicines, not a weight loss shortcut. They reduce blood volume and can lower blood pressure within days to weeks. If you feel lightheaded when standing, or your urine drops a lot, tell your doctor. Also watch for muscle cramps, weakness, or a fast heartbeat — these can be signs of low potassium or other electrolyte shifts.
Safety tips and monitoring
Before you start a diuretic, your provider should check your blood pressure, electrolytes, and kidney function. Those tests should repeat within one to two weeks after a dose change. Don’t mix diuretics with NSAIDs like ibuprofen without advice — NSAIDs can blunt their effect and harm kidneys. Watch salt intake: cutting excessive salt often helps the medicine work better. If you take potassium supplements or salt substitutes, check with your prescriber, especially if you are on a potassium‑sparing agent.
Some people should be careful: pregnant or breastfeeding women, people with severe kidney disease, and those taking lithium or certain heart rhythm medicines. Herbal “water pills” such as dandelion extract can add to drug effects and raise risk of dehydration or electrolyte imbalance.
Typical lab checks measure sodium, potassium and creatinine. Potassium under 3.5 mEq/L is considered low and over 5.0 mEq/L is high; both need attention. Your clinician may lower the dose, add a potassium pill, or switch drugs. People with gout should know thiazides can raise uric acid and trigger attacks. Diuretics can also nudge blood sugar up slightly, so monitor glucose if you have diabetes. Keep an updated medication list and show it at every visit — even common cold pills or herbal remedies matter. Simple habits help too: take most diuretics in the morning to avoid night trips to the bathroom and weigh yourself daily to spot sudden fluid changes. Ask about travel, altitude, and exercise risks.
If you have new swelling, sudden shortness of breath, fainting, extreme thirst, or very low urine output, seek medical care. For most people, diuretics work well and safely when used as directed and monitored. Talk openly with your clinician about side effects and goals — good communication keeps treatment on track.