Second Cancers: What They Are, How They Happen, and What You Can Do
When someone survives cancer, the last thing they expect is to hear the word second cancers, new, distinct tumors that develop after a person has been treated for an initial cancer. Also known as secondary malignancies, these aren’t the original cancer coming back—they’re entirely new cancers, often in a different part of the body, triggered by past treatments, genetics, or lifestyle factors. Many people assume that beating cancer means they’re safe for good. But the truth is, treatments that save lives can sometimes, over time, increase the risk of new cancers.
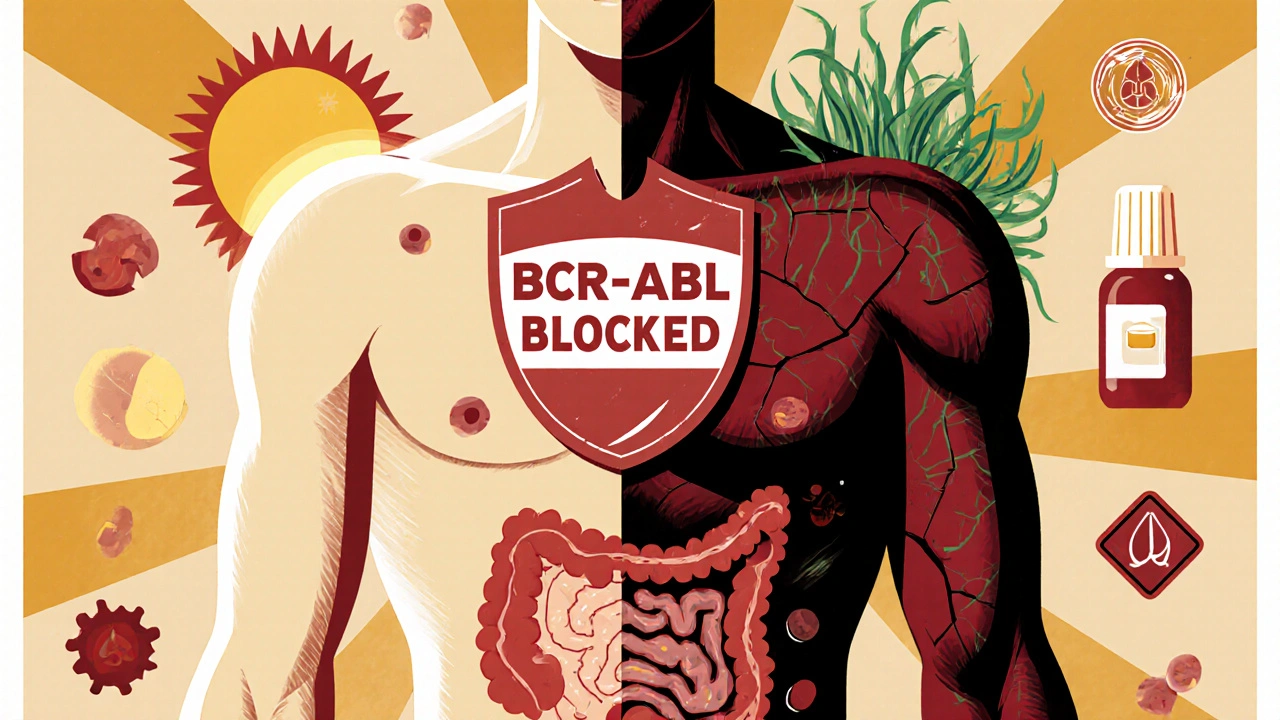
Chemotherapy and radiation don’t just target cancer cells. They can damage healthy DNA in nearby tissues, and that damage can lie dormant for years before turning into a new tumor. For example, women treated for breast cancer with radiation may later develop lung or thyroid cancer. Men treated for prostate cancer with radiation have a higher chance of developing bladder or rectal cancer. Even drugs like alkylating agents or topoisomerase inhibitors, used to kill fast-growing cancer cells, can mess with cell repair systems and lead to blood cancers like leukemia years later. This isn’t common—but it’s real enough that survivors need to know the signs.
It’s not just treatment. Genetics play a role too. If you carry a mutation like BRCA1 or Li-Fraumeni syndrome, your body is already more prone to multiple cancers over time. Add in smoking, poor diet, or lack of screening, and the risk climbs even higher. That’s why follow-up care after cancer isn’t just about checking for recurrence—it’s about catching new cancers early. Regular screenings, like colonoscopies, mammograms, or skin checks, aren’t optional for survivors. They’re part of staying alive.
Some survivors worry that getting treatment was a mistake. But let’s be clear: the benefits of treating the first cancer almost always outweigh the long-term risks. The goal isn’t to scare you—it’s to empower you. Knowing your history, tracking your body, and talking openly with your doctor can make all the difference. The posts below dive into exactly that: real stories, science-backed risks, and practical steps survivors can take to protect themselves. From understanding how certain chemo drugs raise leukemia risk to learning which screenings are most critical after specific treatments, you’ll find clear, no-fluff advice that actually helps.