Food Allergy & Heartburn Trigger Checker
Check your food triggers
This tool helps identify potential food allergy connections to your heartburn based on the article's information about food triggers. For best results, keep a symptom diary for 14 days.
Key Takeaways
- Heartburn can be aggravated by immune reactions to certain foods.
- Not all heartburn is allergy‑related; classic triggers include fatty or spicy meals.
- Identifying a food‑allergy link often requires an elimination diet or professional testing.
- Managing symptoms may involve antihistamines, acid‑reducing meds, and careful meal planning.
- Seek medical advice if pain is frequent, severe, or accompanied by swallowing difficulty.
When you feel that burning sensation behind your breastbone after a meal, you probably think of heartburn a painful reflux of stomach acid into the esophagus. Most people blame spicy sauces, chocolate or coffee, but an often‑overlooked culprit is the body’s immune response to certain foods. Below we untangle how food allergies immune‑mediated reactions that occur when the body mistakenly identifies a food protein as harmful can ignite or worsen that same burning feeling.
What Exactly Is heartburn?
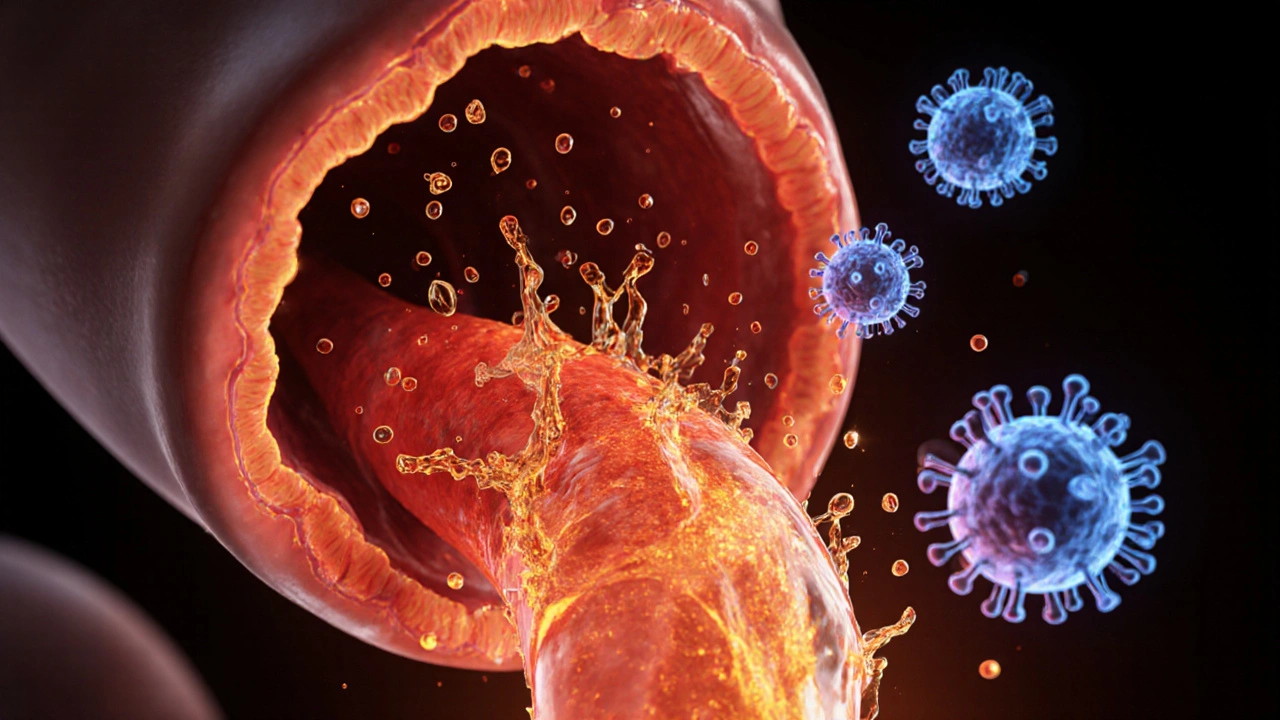
Heartburn is a symptom, not a disease. It happens when the lower esophageal sphincter (LES) relaxes inappropriately, letting acidic stomach contents splash up into the esophageal lining. The lining isn’t built to handle acid, so you feel a sharp, sometimes sour taste and a burning pain that can travel up to the throat.
Clinically, the condition falls under gastroesophageal reflux disease (GERD) a chronic form of reflux that occurs at least twice a week or causes complications. While occasional heartburn is normal, frequent episodes indicate the LES is chronically weak or overloaded.
Food Allergies 101
A food allergy is an immune system the network of cells and proteins that protects the body from harmful substances overreaction. When a person with a food allergy eats the offending food, the body releases histamine a chemical that causes itching, swelling, and other allergy symptoms and other inflammatory mediators. Classic signs include hives, swelling, wheezing, or even anaphylaxis. But the gastrointestinal tract is a frequent battlefield, so symptoms like nausea, abdominal pain, and yes-heartburn-can also surface.

How Food Allergies Can Trigger Heartburn
There are three main pathways linking the two:
- Direct irritation: Some allergens, especially dairy or gluten, contain proteins that irritate the esophageal lining. The irritation can lower the LES pressure, making reflux easier.
- Histamine surge: Histamine not only causes itching but also stimulates stomach acid production. Higher acid levels increase the chance of reflux.
- Eosinophilic esophagitis (EoE): This is a chronic allergic inflammation of the esophagus. In EoE, eosinophils (a type of white blood cell) infiltrate the esophageal tissue, causing narrowing and reflux symptoms. Many patients describe persistent heartburn as their primary complaint.
While the mechanisms differ, the common denominator is that an immune response can weaken the LES or increase acid, both of which spark heartburn.
Common Food Triggers to Watch
| Allergen | Typical reaction | Why it may cause heartburn |
|---|---|---|
| Dairy | Hives, abdominal cramp | Casein can irritate esophageal lining; high fat content slows gastric emptying. |
| Gluten | Diarrhea, bloating | Triggers inflammation in sensitive individuals, potentially lowering LES tone. |
| Shellfish | Swelling, wheeze | Strong histamine release boosts stomach acid. |
| Nuts | Itching, stomach pain | High fat content and potential allergenicity both strain the LES. |
| Soy | Skin rash, gas | Soy proteins can provoke eosinophilic inflammation in the esophagus. |
Identifying an Allergy‑Related Heartburn Pattern
Because many foods can cause reflux even without an allergy, pinpointing the cause requires careful observation:
- Symptom diary: Write down everything you eat, the time you ate it, and any heartburn episodes. Look for repeat patterns within 30‑90 minutes after meals.
- Elimination phase: Remove suspected allergens (e.g., dairy, gluten, shellfish) for two weeks. If heartburn improves, re‑introduce one food at a time to confirm.
- Medical testing: Skin‑prick tests or specific IgE blood tests can verify sensitization. For esophageal issues, an endoscopy with biopsies can diagnose eosinophilic esophagitis.
Managing the Dual Challenge
Dietary Strategies
- Eat smaller, more frequent meals to reduce stomach pressure.
- Avoid lying down for at least three hours after eating.
- Limit high‑fat, fried, and heavily spiced foods that relax the LES.
- Choose low‑acid options: oatmeal, bananas, grilled chicken, and non‑citrus vegetables.
- If an allergy is confirmed, adopt a strict avoidance plan. Many people find success with a gluten‑free or dairy‑free regimen.
Medication Options
Over‑the‑counter antacids (calcium carbonate) or H2 blockers (ranitidine) can neutralize acid temporarily. For chronic GERD, proton‑pump inhibitors (omeprazole) are more effective. If histamine is a major driver, non‑sedating antihistamines (cetirizine) or H1‑blockers may reduce both allergy symptoms and acid output.
Professional Help
When heartburn occurs more than twice a week, or when you notice swallowing difficulty, weight loss, or persistent cough, schedule a gastroenterology appointment. A nutritionist experienced in food‑allergy management can help craft a personalized meal plan.
Quick Checklist for Everyday Relief
- Keep a food‑symptom log for at least 14 days.
- Eliminate common allergens (dairy, gluten, shellfish) for a trial period.
- Raise the head of your bed 6‑8 inches.
- Chew food slowly; avoid carbonated drinks.
- Carry an antacid and an antihistamine if you’ve confirmed a trigger.
When to Seek Immediate Care
If you experience any of the following, treat it as an emergency:
- Severe chest pain that radiates to the arm or jaw (could be heart‑related).
- Difficulty breathing, swelling of lips or tongue.
- Vomiting blood or material that looks like coffee grounds.
- Persistent vomiting or inability to keep fluids down.
These signs may indicate an allergic reaction or a serious complication of reflux that needs prompt medical attention.
Frequently Asked Questions
Can a food allergy cause chronic heartburn?
Yes. Allergic inflammation can lower LES pressure and increase stomach acid, leading to frequent reflux. Conditions like eosinophilic esophagitis are classic examples where an allergic response produces ongoing heartburn.
Is it safe to self‑diagnose a food allergy based on heartburn?
Self‑diagnosis is risky because many foods trigger reflux without an immune reaction. A structured elimination diet and, if possible, allergy testing give a reliable answer.
Do antihistamines help with heartburn?
They can, but only if histamine release is a major factor. For pure acid reflux, acid‑reducing medications work better. Always discuss combined use with a doctor.
What is the difference between gastritis and heartburn?
Gastritis is inflammation of the stomach lining, often causing nausea and upper‑abdominal pain. Heartburn is the sensation of acid flowing back into the esophagus. Both can coexist but stem from different tissue irritation.
Can a gluten‑free diet reduce heartburn?
For people with gluten sensitivity or celiac disease, removing gluten can lower overall inflammation and improve LES function, which may lessen reflux episodes.






Matthew Marshall
October 12, 2025 AT 02:20If my heart were a theater, this article would be the dramatic climax that leaves the audience gasping for breath!
Lexi Benson
October 12, 2025 AT 03:20Oh great, another list of foods that apparently double‑act as heart‑burn saboteurs-just what my dinner plan needed.
Vera REA
October 12, 2025 AT 04:20The article correctly emphasizes that not every bout of heartburn originates from reflux alone. It highlights the immunologic pathways, such as histamine‑mediated acid secretion, which are often overlooked. The distinction between direct irritation and eosinophilic esophagitis is particularly useful for clinicians. Overall, the piece provides a balanced overview of dietary triggers.
John Moore
October 12, 2025 AT 05:20I appreciate the clear breakdown of mechanisms; it helps bridge the gap between allergy science and everyday eating habits. While I’m assertive about encouraging self‑monitoring, I also respect that each individual’s response can vary. Keeping a symptom diary remains the most pragmatic step forward.
Adam Craddock
October 12, 2025 AT 06:20I find the differentiation between histamine‑induced acid secretion and mechanical LES relaxation particularly noteworthy. The article’s recommendation for a structured elimination diet aligns with established clinical protocols. Moreover, the inclusion of professional testing options adds credibility to the approach. It is a concise yet comprehensive guide.
Kimberly Dierkhising
October 12, 2025 AT 07:20From a gastroenterological perspective, the interplay of lipid load and gastric emptying time is a critical factor often omitted in lay discussions. High‑fat foods, such as certain nuts, increase intragastric pressure, thereby exacerbating reflux episodes. Additionally, the cytokine cascade triggered by allergens can modulate smooth muscle tone in the LES. Incorporating jargon like “eosinophilic infiltration” reinforces the pathophysiological depth. Clinicians should consider these nuances when advising patients.
Rich Martin
October 12, 2025 AT 08:20You know, thinking about heartburn as just a pesky reflux is like ignoring the universe's deeper existential angst. When an allergen triggers a histamine surge, it's not merely a chemical reaction; it's the body's way of shouting, 'I am being wronged!' That shout reverberates through the lower esophageal sphincter, loosening its grip like a tired gatekeeper at midnight. And what does that mean for the average person? It means that the burn you feel is a symptom of a hidden war inside your gut. But the war isn’t always obvious-some foods act as silent infiltrators, slipping past your immune radar. Take dairy, for instance; its casein proteins can coat the esophagus, creating a slippery surface that invites acid to splash. Meanwhile, gluten can provoke low‑grade inflammation that subtly erodes LES tone over weeks. Shellfish, with its high histamine content, essentially puts a turbo‑charger on acid production. Nuts, loaded with fat, delay gastric emptying, increasing intra‑abdominal pressure and pushing acid upward. Soy, often overlooked, may trigger eosinophilic esophagitis, a chronic allergic inflammation that narrows the esophageal lumen. All these mechanisms converge on a single outcome: a weakened barrier and an overactive acid factory. The practical upshot? A systematic elimination diet isn’t just a fad; it’s a strategic retreat to reclaim control. Start by cutting out the high‑probability culprits for two weeks, then re‑introduce one at a time while logging every flicker of burn. If the heartburn subsides, you’ve identified a trigger; if not, you keep searching, because the gut is an intricate puzzle. And remember, medication can mask the symptoms, but it won’t teach your immune system to stop overreacting. So, embrace the patience of a philosopher and the rigor of a scientist, and you’ll eventually map the hidden connections.
Buddy Sloan
October 12, 2025 AT 09:20That sounds really tough, and I’m sorry you’re dealing with that fire in your chest 😔.
SHIVA DALAI
October 12, 2025 AT 10:20In the grand drama of digestion, every allergen assumes the role of a villain intent on stealing the peace of the esophagus.
The article masterfully scripts the conflict, guiding readers toward a triumphant resolution.
Vikas Kale
October 12, 2025 AT 11:20From a pathophysiological standpoint, the synergistic effect of histamine release and reduced lower esophageal sphincter tone creates a perfect storm for gastro‑esophageal reflux. The kinetic profile of dairy‑derived casein prolongs mucosal exposure to acidic content, while gluten‑induced cytokine activation subtly impairs neuromuscular coordination. Shellfish, rich in histidine, serves as a precursor for endogenous histamine, effectively amplifying gastric hydrochloric secretion. Lipid‑dense nuts elevate post‑prandial gastric volume, increasing intra‑abdominal pressure and promoting retrograde flow. Soy proteins have been implicated in eosinophilic esophagitis, adding an inflammatory dimension that narrows the lumen and augments reflux severity.
Deidra Moran
October 12, 2025 AT 12:20Sure, all these "scientific" recommendations are just a distraction while big pharma pushes us toward endless prescriptions. The real agenda is to keep us dependent on medication, not to solve the underlying immune manipulation. Look beyond the surface and you’ll see the pattern.
Zuber Zuberkhan
October 12, 2025 AT 13:20I hear your concerns, but let’s keep the conversation constructive and focus on evidence‑based steps anyone can try. Starting with a simple elimination of dairy and gluten can provide real insight without costly interventions. We’re all here to support each other’s health journeys.
Tara Newen
October 12, 2025 AT 14:20Honestly, most people just need to stop over‑thinking and follow the basic guidelines. If you’re not willing to make simple changes, the problem will persist.
Amanda Devik
October 12, 2025 AT 15:20Take heart! The path to relief may seem steep but every small step shines brighter than the last.