Skin Itch Trigger Identifier
Potential Triggers Identified
Key Takeaways
- Identify the most common causes of itch in seniors before reaching for medication.
- Use gentle, fragrance‑free moisturizers at least twice daily to rebuild the skin barrier.
- Non‑drug measures-cool compresses, proper clothing, and humidity control-often provide enough relief.
- When itching is intense, persistent, or linked to systemic illness, involve a health professional promptly.
- Keep a simple diary to track triggers, treatments, and improvement over time.
When an older loved one keeps scratching, it’s more than a nuisance-persistent itching can signal deeper health issues. Pruritus in elderly is a chronic sensation that triggers the urge to scratch and often stems from age‑related skin changes, medical conditions, or medications. Understanding why it happens is the first step toward relief.
Why Does Itch Become a Bigger Problem After 65?
Skin naturally thins with age, producing less natural oil and a weaker barrier. This condition, called xerosis(dry skin) that commonly affects older adults, leading to tight, flaky, and itchy skin, creates a perfect storm for pruritus. Add to that the higher likelihood of chronic diseases-diabetes, kidney or liver impairment, and thyroid disorders-each of which can trigger itch through internal inflammation or toxin buildup.
Medications amplify the risk. Many seniors take antihypertensives, statins, or opioid pain relievers, all of which list “pruritus” as a possible side effect. The cumulative effect of multiple drugs (polypharmacy) can irritate nerve endings and make the skin hypersensitive.
Common Triggers to Watch For
- Dry skin (xerosis): The most frequent cause; worsens in low‑humidity seasons.
- Medication adverse effects: especially antihistamines, diuretics, and antidepressants.
- Systemic illnesses: chronic kidney disease, liver cirrhosis, and uncontrolled diabetes.
- Environmental factors: hot showers, harsh soaps, wool or synthetic fabrics.
- Skin conditions: eczema, psoriasis, or fungal infections that may coexist.
Assessing Severity and When to Call a Doctor
Not every itch needs a prescription, but certain signs demand professional attention:
- Itch that wakes the person at night or leads to visible skin damage.
- Rapid spread, redness, or swelling suggesting infection.
- Associated systemic symptoms-fever, weight loss, jaundice, or swelling of the ankles.
- Persistent itch despite daily moisturising and simple home measures for more than two weeks.
If any of these appear, schedule a visit with a primary‑care physician or dermatologist. They may order blood tests (creatinine, liver enzymes, glucose) to rule out underlying organ dysfunction.
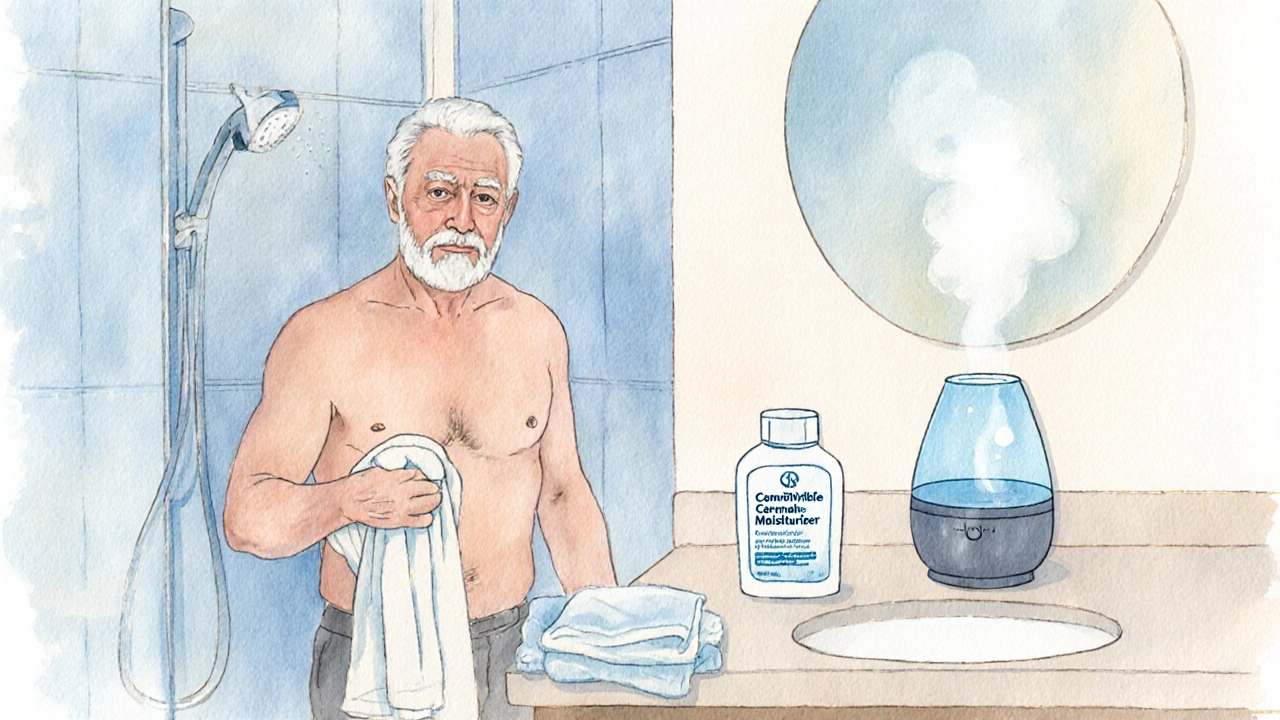
Non‑Pharmacologic Strategies That Work
Before reaching for pills, try these skin‑friendly habits. They require little cost and have minimal side effects.
- **Moisturise immediately after bathing.** Pat the skin dry, then apply a generous layer of a fragrance‑free moisturiserdesigned for sensitive or dry skin, preferably with ceramides, glycerin, or petrolatum. Reapply every 2-3hours during flare‑ups.
- **Cool compresses.** A cool, damp washcloth for 5‑10 minutes reduces nerve firing and provides instant calm.
- **Adjust bathing habits.** Use lukewarm water, limit showers to 10minutes, and choose mild, sulfate‑free cleansers.
- **Control indoor humidity.** Aim for 40‑60% humidity with a humidifier, especially in winter.
- **Choose breathable clothing.** Cotton or bamboo fibers reduce friction and sweat buildup.
Choosing the Right Moisturiser: A Quick Comparison
| Type | Key Ingredient | Texture | Best For | Pros | Cons |
|---|---|---|---|---|---|
| Occlusive | Petrolatum | Thick, greasy | Very dry, cracked skin | Creates a seal that locks moisture in for 12‑24hrs | May feel heavy; not ideal for daytime use under clothes |
| Humectant | Glycerin | Light, watery | Normal‑to‑dry skin needing quick hydration | Absorbs quickly, can be layered | Relies on external humidity; can feel sticky in dry air |
| Emollient | Lanolin or shea butter | Creamy | Combination dry‑sensitive skin | Softens skin, reduces roughness | Potential allergen for lanolin‑sensitive individuals |
Pharmacologic Options When Home Care Isn’t Enough
If itch persists despite diligent moisturising, short‑term medication can bridge the gap.
- Antihistamines (e.g., cetirizine, diphenhydramine). They block histamine, a common itch mediator. Use caution with sedating varieties at night.
- Topical corticosteroids (low‑potency hydrocortisone 1%). Apply a thin layer to inflamed patches for up to 7days. Longer use can thin skin further, so follow medical advice.
- Calcineurin inhibitors (tacrolimus ointment) for those who can’t tolerate steroids; they reduce inflammation without causing atrophy.
- Prescription oral medications such as gabapentin or pregabalin for neuropathic itch associated with renal disease.
Always discuss dosing with a healthcare provider, especially because older adults metabolise drugs more slowly and may experience side effects.

Creating an Itch‑Management Routine
Turn the tips into a repeatable daily schedule. Consistency beats occasional effort.
- Morning: Quick lukewarm shower → pat dry → apply occlusive moisturiser (petrolatum‑based).
- Mid‑day: Re‑apply a humectant lotion if skin feels tight.
- Evening: Use a gentle cleanser → cool rinse → apply emollient cream → if itching continues, add a short‑acting antihistamine.
- Before bed: Cool compress for 5minutes → low‑dose sedating antihistamine if needed.
Keep a small notebook beside the bedside to note:
- What triggered the itch (new soap, weather change, medication start).
- Which moisturiser gave the best relief.
- Any side effects from medication.
Review the log with a caregiver or clinician every few weeks.
When to Consider Specialist Referral
Even with the best home plan, some cases need a dermatologist or geriatric specialist.
- Persistent itch with no identifiable trigger after 4weeks.
- Signs of secondary infection: oozing, crusting, foul odor.
- Suspicion of systemic disease (elevated liver enzymes, uremic itch).
- Need for advanced therapies such as phototherapy or biologics.
Caregiver Checklist
- Inspect skin daily, especially in folds and feet.
- Maintain a fragrance‑free environment; avoid scented lotions or detergents.
- Rotate moisturisers if skin becomes accustomed to one type.
- Monitor medication list for new drugs that list itch as a side effect.
- Ensure adequate fluid intake - dehydration worsens dryness.
- Schedule regular health check‑ups to screen for diabetes, kidney, or liver disease.
Frequently Asked Questions
Why does my mother’s skin feel itchier during winter?
Cold, dry air strips moisture from the outer skin layer, worsening xerosis. Using a humidifier and applying an occlusive moisturiser right after bathing can counteract the loss.
Can over‑the‑counter antihistamines be used safely for seniors?
Yes, but start with a low dose and prefer non‑sedating options like cetirizine. Sedating antihistamines (e.g., diphenhydramine) should be reserved for nighttime and used sparingly because they can increase fall risk.
My father has chronic kidney disease and constant itch. What helps?
Uremic pruritus often responds to topical moisturisers, cool compresses, and sometimes oral gabapentin under doctor supervision. Controlling phosphorus levels through diet also reduces itching episodes.
Is it risky to use petroleum‑based ointments on thin elderly skin?
Petrolatum is safe and effective; it creates a barrier that prevents water loss. The only caution is to apply a thin layer to avoid a feeling of greasiness and to keep the skin clean to prevent bacterial overgrowth.
What lifestyle changes reduce itch for people with diabetes?
Maintain good blood‑sugar control, keep feet clean and dry, wear cotton socks, and moisturise daily. Neuropathic itch improves with gabapentin if standard measures fail.







surender kumar
October 10, 2025 AT 20:54Oh, so we’re supposed to just slap on a cheap lotion and call it a day? As if senior skin isn’t a battlefield of dryness, medication side‑effects, and systemic disease. Sure, moisturise, but don’t ignore the fact that many of these elders are on a cocktail of diuretics and statins that actually exacerbate pruritus. And let’s not pretend that a “cool compress” isn’t a band‑aid for deeper metabolic woes. If you’re not checking kidney and liver panels, you’re essentially playing doctor with a blindfold.
JOJO Yang
October 15, 2025 AT 04:54Yo! This guide is like, super helpful but also kinda missing the point. Like, u gotta remember to use a fragrance‑free cream, right? And dont forget to howi d the water temperature – not too hot! Also, i think a bit more on krim for night‑time would be nice. Typos aside, good job!
Faith Leach
October 19, 2025 AT 12:54Everyone loves to talk about moisturisers and humidifiers while the real culprits are hidden behind the curtain of corporate medical conspiracies. The pharmaceutical industry pushes opioids and antihistamines as miracle solutions, but they mask the underlying truth: that our elders are being drugged into compliance. They claim it’s “pruritus” from kidney disease, yet never disclose how many of those patients are on secretive, unapproved compounds that increase nerve sensitivity. Ever notice how the same brands that sell “skin‑softening” creams also fund the studies that downplay side‑effects? It’s a systematic effort to keep the population dependent on consumer products while ignoring the systemic toxins. Governments collude, using tax dollars to subsidise these products, ensuring there’s no real investigation into environmental pollutants that trigger itching. They control the narrative through “expert” articles that sound scientific but are just marketing fluff. The humidity control devices you mention are often manufactured by the same conglomerates that sell the moisturisers – a perfect feedback loop. When they say “consult a healthcare professional”, they’re really pushing you toward a doctor who’s paid off. Even the recommended “cool compress” is a euphemism for a cheap gadget sold by the same corporation that sponsors the guide. And let’s not forget the role of 5G towers and EMF exposure, which are increasing in frequency across senior living facilities, causing dermal irritation that no one talks about. The truth is that real relief comes from rejecting the entire pharma‑propaganda and focusing on natural, non‑commercial interventions – like oat baths, balms made from locally sourced bee pollen, and simply reducing exposure to synthetic chemicals. So while you zip through the list of moisturisers, remember the bigger picture: it’s not the skin that’s the problem, it’s the system that’s trying to sedate and silence the elderly.
Kate Babasa
October 23, 2025 AT 20:54In the context of geriatric dermatology, it is paramount to integrate evidence‑based protocols whilst maintaining patient‑centred communication; therefore, employ a multimodal approach, encompassing barrier restoration, environmental modulation, and pharmacologic adjuncts. The utilisation of occlusive agents, such as petrolatum, constitutes a foundational pillar; however, the selection must be predicated upon individual lipid profile and tolerability thresholds. Moreover, humidity regulators should be calibrated to a range of 40‑60 %, optimizing epidermal hydration without fostering microbial overgrowth. It is advisable to schedule moisturiser application post‑bath, within a temporal window of two minutes, to maximise transepidermal water loss (TEWL) mitigation. Consistency in routine engenders dermal resilience, thereby attenuating pruritic episodes.
Crystle Imrie
October 28, 2025 AT 03:54Honestly, slapping on a cream isn’t a miracle, but it’s better than nothing.
Shelby Rock
November 1, 2025 AT 11:54One could argue that the philosophical underpinnings of skin health reflect a broader existential equilibrium; when the barrier is compromised, the self is unsettled. Yet practical steps-like choosing a ceramide‑rich ointment and avoiding harsh surfactants-are where theory meets day‑to‑day life. Misspelling aside, the core idea is simple: protect, hydrate, and observe.
Alex Iosa
November 5, 2025 AT 19:54While the guide offers a reasonable overview, it omits a crucial element: the systematic review of patient medication lists to identify iatrogenic pruritus. A thorough audit of antihypertensives, statins, and opioids is indispensable before initiating topical therapy.
melissa hird
November 10, 2025 AT 03:54Ah, the ever‑so‑comprehensive treatise on elderly itching-truly a masterpiece of modern nursing literature. One can only marvel at the depth of insight presented, albeit presented with the subtlety of a marching band. Nonetheless, the recommendations are sound, if you enjoy being lectured.
Mark Conner
November 14, 2025 AT 11:54Look, we’ve got to protect our own folks. The government doesn’t care about that itchy old man next door, so it’s up to us to keep the skin tight and the meds in check.
Charu Gupta
November 18, 2025 AT 19:54Great post! 🎉 Very thorough, and I especially appreciate the reminder about checking for infections. 👍
Abraham Gayah
November 23, 2025 AT 03:54Wow, another guide about skin… yawn.
rajendra kanoujiya
November 27, 2025 AT 11:54Sure, whatever.
Caley Ross
December 1, 2025 AT 19:54I’m just observing that most people overlook the simple step of applying moisturizer right after pat‑drying. It’s a low‑effort, high‑reward habit.
Bobby Hartono
December 6, 2025 AT 03:54It’s really important to foster an environment where caregivers feel empowered to be proactive about skin health. First, we should emphasize daily visual inspections-especially in skin folds, behind the ears, and on the feet-since these areas are prone to moisture accumulation and subsequent maceration. Second, we need to advocate for fragrance‑free household products; even “natural” scented soaps can contain essential oils that irritate sensitive epidermis. Third, the hydration of the skin is directly linked to systemic hydration: encouraging regular water intake, unless contraindicated by cardiac issues, can make a noticeable difference. Fourth, rotating moisturisers prevents the skin from developing tolerance; a switch between occlusive (petrolatum‑based) and humectant (glycerin‑based) products can keep the barrier dynamic. Fifth, education on proper bathing practices-lukewarm water, short duration, and gentle, sulfate‑free cleansers-cannot be overstated. Sixth, for those on polypharmacy regimens, a medication review with a pharmacist can identify culprits such as antihistamines with anticholinergic effects that paradoxically dry the skin further. Seventh, nocturnal itching may be mitigated by a low‑dose, non‑sedating antihistamine taken an hour before bedtime, but only under professional guidance to avoid falls. Eighth, incorporating a simple diary-perhaps a one‑page template next to the bedside lamp-helps track triggers, interventions, and outcomes, providing valuable data for clinicians. Ninth, we must not forget the psychosocial impact; itching can lead to anxiety and sleep deprivation, so a calm, supportive atmosphere is essential. Finally, when signs of infection appear-redness, warmth, purulent discharge-prompt medical evaluation is critical to avoid cellulitis or sepsis. By combining these practical steps with compassion, we can significantly improve quality of life for our elderly loved ones.
George Frengos
December 10, 2025 AT 11:54Great advice! Keeping the routine simple and consistent really does make a difference for seniors. Thanks for the detailed steps.
Jonathan S
December 14, 2025 AT 19:54While the guide’s recommendations are a decent starting point, it’s essential to recognize the limitations of over‑generalization. Applying a one‑size‑fits‑all moisturiser overlooks individual variations in lipid composition and microbiome health. Moreover, the emphasis on “cool compresses” fails to address the underlying neuropathic mechanisms that contribute to pruritus in renal failure patients. A more nuanced approach would incorporate sensory testing and possibly low‑dose gabapentinoids under supervision. 🍃😊
Charles Markley
December 19, 2025 AT 03:54In the realm of dermatologic therapeutics, the discourse often neglects the psychoneuroimmunological axis, a critical factor in geriatric pruritus. By confining recommendations to topical agents and environmental controls, we risk perpetuating a reductionist paradigm that marginalizes the complex biopsychosocial interplay. Consequently, a multidisciplinary framework-integrating neurology, psychiatry, and gerontology-is paramount for efficacious management.
L Taylor
December 23, 2025 AT 11:54Nice guide! It’s friendly and clear without being too wordy.
Matt Thomas
December 27, 2025 AT 19:54Honestly, the advice is fine but you’ve got to check the meds list first-most of the time, the itching is iatrogenic.