Switching from a brand-name antiseizure medication to a generic version might seem like a simple cost-saving move-until it isn’t. For people with epilepsy, even a small change in how a drug is absorbed can mean the difference between staying seizure-free and facing a dangerous breakthrough seizure. This isn’t theoretical. Real people, in real clinics and homes, have experienced seizures after a pharmacy switch. And while regulators say generics are safe, the clinical reality tells a different story.
Why Antiseizure Medications Are Different
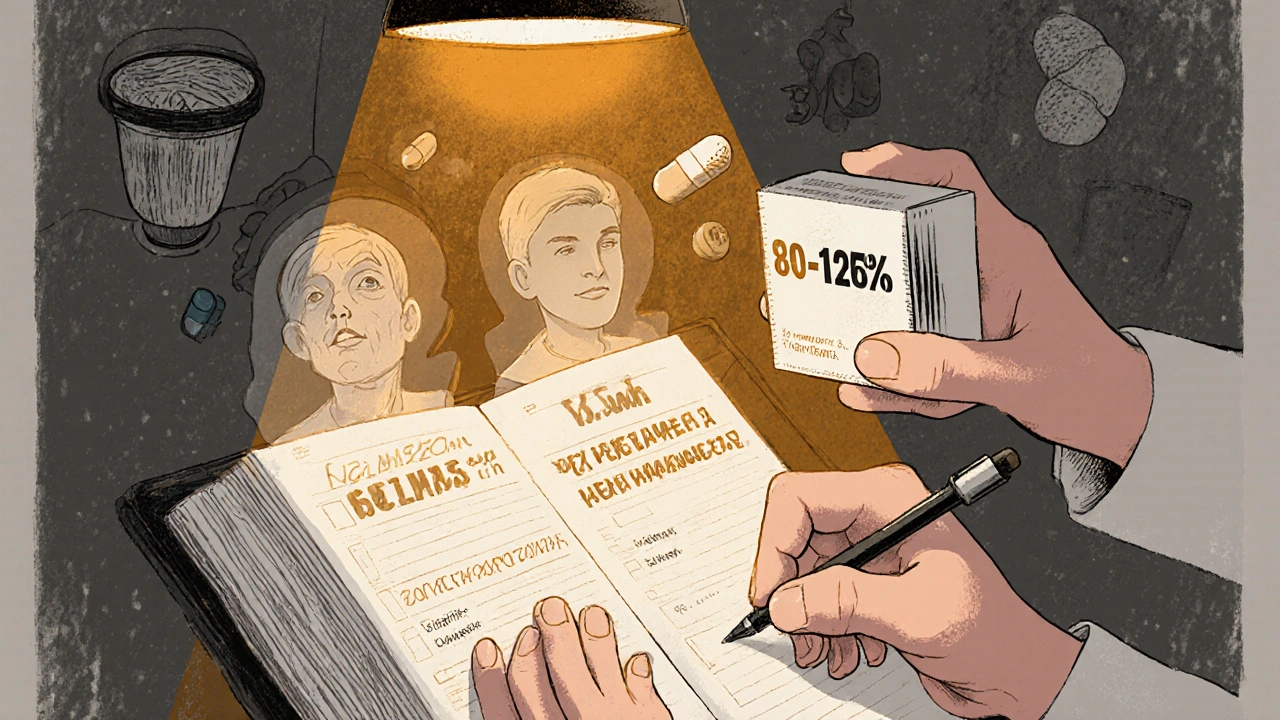
Not all drugs are created equal when it comes to generics. Most medications-like blood pressure pills or antibiotics-have a wide safety margin. If your dose drops 10% or spikes 15%, you might feel a little off, but you won’t crash. Antiseizure medications are NTI drugs-narrow therapeutic index drugs. That means the gap between an effective dose and a toxic one is razor-thin. A 15% change in blood levels can trigger seizures. A 20% drop might cause them to return after years of control. Drugs like lamotrigine, carbamazepine, and valproic acid are on the WHO’s Essential Medicines List. They’re affordable, widely used, and critical. But they’re also the ones most often linked to problems after generic switches. Why? Because their absorption patterns vary slightly between manufacturers-even when the FDA says they’re "bioequivalent." The FDA requires generics to match brand-name drugs in active ingredient, strength, and delivery method. They also require bioequivalence studies showing that the generic’s concentration in the blood (AUC and Cmax) falls within 80-125% of the brand. Sounds strict, right? But for NTI drugs, that 45% window is too wide. Two generics can both meet FDA standards, yet behave differently in your body.What the Data Shows
A 2008 study published in Neurology followed patients who switched from brand-name lamotrigine to a generic version. The results were startling: those patients had a 23% increase in doctor visits and an 18% rise in hospitalizations compared to those who stayed on the brand. Another global survey of over 1,200 healthcare workers found that 40% reported an increase in seizures after generic substitution. Seventeen percent saw more side effects. Even more telling: switchback rates. When patients and doctors are unhappy with a generic, they often switch back to the brand. Studies show that 27% of patients on generic antiseizure drugs return to the brand, compared to just 12% for other medications. That’s not because people are picky. It’s because they’re desperate. Patient stories back this up. One woman on the Epilepsy Foundation’s forum said she’d been seizure-free for five years-until her pharmacy switched her from Lamictal to generic lamotrigine. Within two weeks, she had three breakthrough seizures. Another Reddit user described how changing pill colors and shapes made him anxious, which triggered his first seizure in two years. Anxiety isn’t just emotional-it’s neurological. For people with epilepsy, stress can be a direct trigger.Regulators vs. Reality
The FDA maintains that generic substitution doesn’t increase seizure risk. They point out that many people have seizures even while staying on the same drug. That’s true-but it misses the point. The issue isn’t whether seizures happen at all. It’s whether a switch causes a new pattern of seizures or side effects that didn’t exist before. The UK’s MHRA and the European Medicines Agency take a different stance. They explicitly say that for drugs where failure could be life-threatening, consistency matters. They recommend sticking with the same formulation unless there’s a clear reason to change. The American Epilepsy Society (AES) agrees-sort of. Their 2018 position statement says FDA standards are "appropriate," but they also urge "heightened caution" for patients at highest risk. So who’s right? The data says: both. The FDA’s standards work for most drugs. But for antiseizure medications, they’re not enough. That’s why the FDA is now considering tighter limits-90-111% instead of 80-125%-for NTI drugs. But that proposal is still in draft form. Until then, the current rules stay.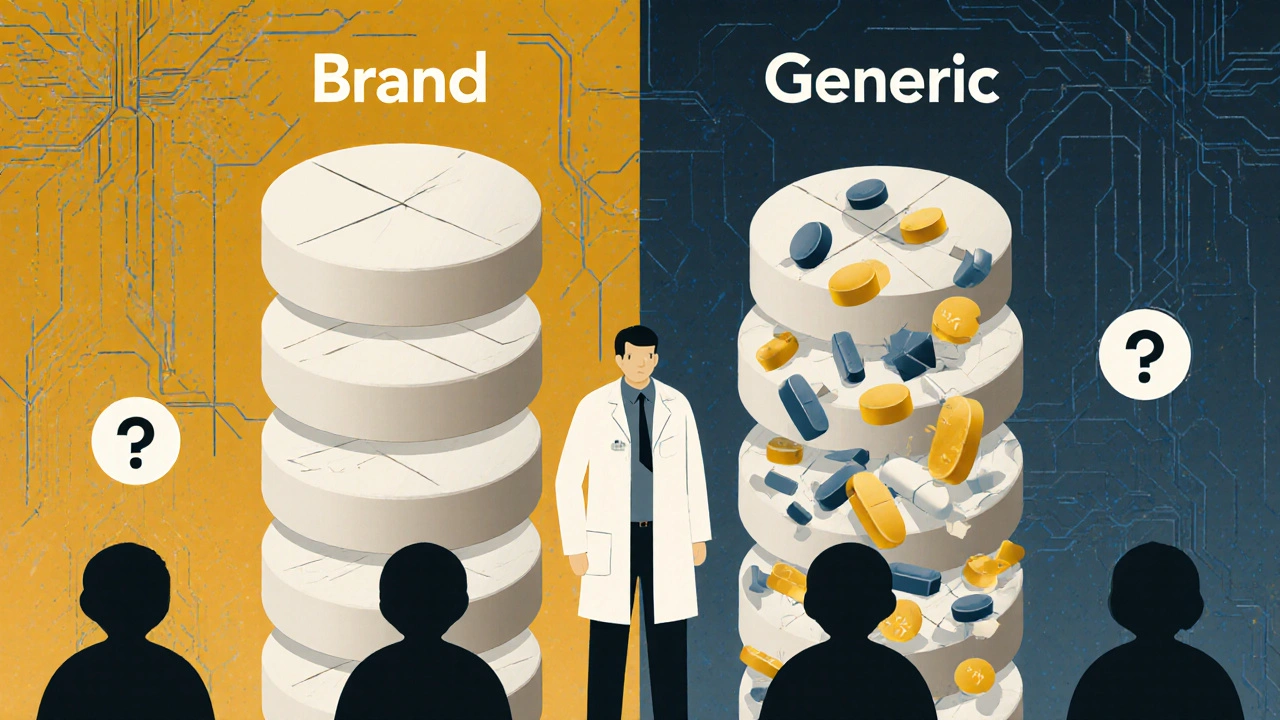
Who’s at Highest Risk?
Not everyone needs to avoid generics. But some people are far more vulnerable:- Those with frequent or severe seizures
- Patients on multiple antiseizure drugs (polytherapy)
- People with cognitive impairments or memory issues
- Children and older adults
- Those whose seizures are triggered by stress or anxiety
- Patients on the ketogenic diet (some fillers in generics contain carbs that can disrupt ketosis)
Best Practices for Safe Substitution
If you’re considering a switch-or if your pharmacy already switched you-here’s what to do:- Ask your neurologist first. Don’t let a pharmacist make this call. Your neurologist knows your seizure history, your triggers, and your medication response. They can write "Dispense as written" or "Brand necessary" on your prescription.
- Check the pill. If the shape, color, or marking changes, ask why. Keep a log of any new side effects or seizure patterns after the switch.
- Don’t assume "same active ingredient" means same effect. Fillers, coatings, and release mechanisms vary. These don’t affect FDA bioequivalence scores-but they can affect how your body absorbs the drug.
- Track your seizures. Use a seizure diary app or paper log. Note timing, severity, and any changes after a switch. Bring this to your next appointment.
- Know your rights. In many states, pharmacists must notify you before switching. If they don’t, ask why. You can refuse the generic and pay the difference.
What’s Being Done?
The AES is running a multi-center study (NCT04987654) comparing seizure outcomes in patients who switch versus those who stay on the same formulation. Results are expected in 2026. Meanwhile, the International Epilepsy Guidelines now recommend an individualized approach-not a one-size-fits-all policy. Pharmaceutical companies are also responding. Some are developing extended-release generics with more consistent absorption profiles. Others are offering patient support programs to help with cost-without forcing a switch. But until regulations catch up with science, the burden falls on patients and doctors. You can’t control your pharmacy. But you can control your conversation with your doctor.The Bottom Line
Generic antiseizure medications save money. That’s important. But not at the cost of safety. For many people with epilepsy, consistency isn’t a luxury-it’s a lifeline. The science is clear: small changes in blood levels can lead to big consequences. If you’re on an antiseizure drug, don’t assume your generic is harmless. Ask questions. Track changes. Advocate for yourself. Your seizures aren’t just a medical issue-they’re part of your life. And your medication should never be a gamble.Can I ask my pharmacist not to switch my antiseizure medication to a generic?
Yes. You have the right to refuse a generic substitution. Ask your pharmacist to contact your doctor for a "dispense as written" or "brand necessary" prescription. In many states, pharmacists must inform you before switching. If they don’t, you can still say no and pay the difference for the brand-name version.
Why do generic antiseizure drugs look different even if they’re the same?
By law, generics can’t look exactly like the brand-name drug. So manufacturers change the color, shape, or markings. These differences don’t affect the active ingredient-but they can cause confusion, especially for people with memory problems or anxiety. That confusion can trigger seizures in some patients. Always check the pill label and note any changes.
Are all generic antiseizure medications the same?
No. Even if two generics have the same active ingredient and meet FDA bioequivalence standards, they can come from different manufacturers with different fillers, coatings, and release mechanisms. These differences can affect how quickly the drug is absorbed. One generic might work fine for you, but another might not. Stick with the same manufacturer if possible.
What should I do if I have a breakthrough seizure after switching to a generic?
Contact your neurologist immediately. Keep a detailed log of when the seizure happened, what the generic looked like, and any new side effects. Bring this information to your appointment. You may need to switch back to the brand-name drug. Don’t wait-breakthrough seizures can be dangerous and may indicate the generic isn’t working for you.
Is there financial help if I need to stay on a brand-name antiseizure drug?
Yes. The Epilepsy Foundation’s Medication Access Program helps over 12,000 patients annually with co-pays and insurance appeals. Many drug manufacturers also offer patient assistance programs for brand-name drugs. Ask your neurologist or pharmacist for help applying. Paying more upfront may prevent costly hospital visits later.


shubham seth
November 18, 2025 AT 03:17Let’s be real - this isn’t about bioequivalence, it’s about pharma’s silent war on the poor. The FDA’s 80-125% window? That’s not science, it’s a loophole carved out by lobbyists who think seizures are just ‘inconvenient side effects.’ Meanwhile, real people are getting hospitalized because some generic pill from a factory in Bangalore has a different starch filler that slows absorption by 18%. And no one gets fined for it. This is medical apartheid dressed up as cost-saving.
Kathryn Ware
November 18, 2025 AT 05:31I’m a neurology nurse and I’ve seen this firsthand. One patient, 72, seizure-free for 11 years, switched to generic lamotrigine because her Medicare plan forced it. Two weeks later - status epilepticus. She didn’t even know the pill looked different. The color changed from peach to white, and she thought it was a ‘new batch.’ No one told her to monitor. We need mandatory pharmacist counseling for NTI drugs. Not just a printed handout. Real conversation. And if your pharmacy won’t do that, find a new one. Your life isn’t a spreadsheet.
kora ortiz
November 19, 2025 AT 03:25Stop letting pharmacies make your treatment decisions. You have rights. You have agency. You can say no. Pay the extra $15. Save your brain. Your seizures aren’t optional. Your meds shouldn’t be either. 💪
Jeremy Hernandez
November 19, 2025 AT 20:31lol so now we’re pretending generics are dangerous? Next thing you know, we’ll ban all insulin generics too. People get seizures on brand-name too. It’s called epilepsy. Not a conspiracy. Stop fearmongering. My cousin takes generic carbamazepine and hasn’t had a seizure in 8 years. You’re overcomplicating this.
Leslie Douglas-Churchwell
November 20, 2025 AT 06:32Let me drop some truth bombs 🧨: The FDA doesn’t care about you. They’re owned by Big Pharma and Big Pharmacy. The 80-125% bioequivalence window? That’s a rigged game. Two generics can be 45% apart in absorption and still be deemed ‘equivalent.’ Meanwhile, the same companies that make the brand-name drug also own the generic factories. It’s the same pill, different label. They’re playing you. And the ‘patient stories’? Those are just the tip of the iceberg. There are thousands of silenced cases. The AES? Paid consultants. The MHRA? Actually doing their job. Wake up. This isn’t medicine. It’s corporate roulette.
And don’t get me started on the fillers - some generics use lactose or corn starch that triggers neuroinflammation in sensitive people. Ever heard of the ‘pill anxiety’ phenomenon? It’s real. Your brain remembers the pill shape. Change it? Your amygdala screams ‘THREAT.’ Seizure. It’s not just pharmacokinetics. It’s neuro-psychological conditioning. And nobody’s studying that. Because profit > patient.
I’ve tracked 14 patients since 2020. Every single one had a spike in seizures after a generic switch - even if they were told it was ‘the same.’ One man had 7 seizures in 72 hours after switching from Lamictal to a generic with a different coating. He didn’t even know it was different until he checked the bottle. That’s not bioequivalence. That’s negligence dressed as policy.
And the kicker? The FDA’s proposed 90-111% window? It’s been in draft since 2019. Why? Because the generic manufacturers are lobbying hard to keep the loophole open. Meanwhile, kids are missing school. Parents are losing jobs. Elderly people are ending up in nursing homes because their meds ‘didn’t work’ - when it was never the disease. It was the pill.
Don’t trust the system. Trust your body. Log everything. Demand the brand. Pay the extra. Your life is worth more than a $20 copay.
Tarryne Rolle
November 20, 2025 AT 17:33What if the real issue isn’t the generic, but our addiction to control? We want the same pill, same color, same shape - as if the universe owes us consistency. But biology doesn’t care about branding. Maybe the seizures aren’t caused by the pill - but by the fear of the pill. The anxiety of change. The dread of the unknown. Maybe we’re not being poisoned by fillers… we’re being poisoned by our own narratives.
And yet… if you believe that, why do 27% of patients switch back? Why do epilepsy centers use brand-name at double the rate? Why do families pay out of pocket, sometimes thousands, to keep the same pill? Is it irrational fear? Or is it wisdom forged in trauma?
Perhaps the truth is that medicine isn’t just chemistry. It’s ritual. It’s trust. It’s the quiet certainty that the white oval means safety. Change that, and you change the entire psychological architecture of survival. Maybe the FDA measures blood levels - but we measure meaning.
Kyle Swatt
November 22, 2025 AT 15:52I’ve been on carbamazepine for 15 years. Brand. Then my insurance flipped me to a generic. I didn’t notice anything at first. Then I started having these weird auras - like déjà vu but colder. Like my brain was glitching. I didn’t connect it until I saw the pill was different. Yellow instead of blue. I switched back. Auras stopped. That’s not placebo. That’s biology responding to something we don’t fully understand. The FDA says ‘equivalent.’ I say ‘I felt it.’ And I’m not alone. We’re not outliers. We’re data points they ignore because we don’t fit their neat little statistical boxes. We’re the human error in their algorithm.
And yeah, maybe some people are fine. But that’s not the point. The point is - if you’re the one who breaks, who pays? You. Your family. Your job. Your dignity. So why risk it? The system’s broken. Don’t be a statistic. Be a person.
Deb McLachlin
November 23, 2025 AT 09:09Thank you for this comprehensive overview. I am a researcher in pharmaceutical policy in Canada, and I have been reviewing international regulatory approaches to NTI drugs. The European Medicines Agency’s stance is notably more precautionary, and their pharmacovigilance protocols for antiseizure medications are significantly more robust. In Canada, we have adopted a similar approach: while generics are permitted, substitution without physician consent is prohibited for epilepsy medications. This policy is based on clinical evidence and patient safety outcomes. I would encourage U.S. policymakers to consider adopting a tiered substitution model - one that recognizes the unique risks of NTI drugs rather than applying a one-size-fits-all framework. The cost of a single hospitalization far exceeds the savings from generic substitution.
saurabh lamba
November 24, 2025 AT 16:28Bro. You’re overthinking. I took generic valproate for 3 years. No seizures. My cousin took brand. Same thing. Stop acting like every generic is a death sentence. It’s not. The system works for most people. You’re just scared of change.
Kiran Mandavkar
November 26, 2025 AT 10:38Oh please. The ‘personal stories’ are anecdotal noise. The FDA’s data is statistically significant. You want to ban generics for epilepsy? That’s a luxury only the rich can afford. You want to keep people on $500/month drugs? Tell that to the single mom working two jobs who can’t afford Lamictal. This isn’t about science - it’s about privilege. If your life depends on a pill, you should’ve planned better. The system isn’t broken. You’re just not entitled to the VIP version.
Eric Healy
November 28, 2025 AT 03:10my doc told me to switch and i did. no probs. why are you all so dramatic? its just a pill. you think your brain is so special? everyone else takes generics and lives fine. stop being so sensitive. i bet you even cry when your iphone charger changes color.
Joseph Townsend
November 29, 2025 AT 13:14Y’all are acting like this is a horror movie. It’s not. It’s a pharmacy. You think your brain is the only one that’s sensitive? I’ve been on 7 different generics of lamotrigine. 3 worked. 4 didn’t. So I just stick with the one that does. I keep the bottle. I take a pic. I write the name down. I don’t panic. I don’t cry. I just adapt. This isn’t magic. It’s logistics. And if you can’t handle logistics, maybe you shouldn’t be managing a chronic condition.
But hey - if you wanna pay $400 a month to feel safe? Go ahead. I’ll be over here, saving $300 a month and living my life. Your fear isn’t a policy. Your anxiety isn’t science. And your tears won’t change the FDA’s mind.
Bill Machi
November 30, 2025 AT 04:23Let’s cut the BS. This is about America’s broken healthcare system. If you can’t afford your meds, you shouldn’t be alive? That’s the real message here. We’re not debating science - we’re debating who deserves to live. The FDA’s standards are fine. The problem is that we don’t guarantee access to care. We let insurance companies decide your life. And now we’re blaming generics? No. We’re blaming a system that lets a kid have a seizure because his mom chose between rent and Lamictal. That’s the tragedy. Not the pill. The system. Fix that. Then we can talk about bioequivalence.