Imagine looking at a loved one’s face and not being able to make out their eyes. Or trying to read the clock on the wall, but the numbers are blurry, broken, or missing in the middle. This isn’t a trick of the light - it’s age-related macular degeneration, or AMD, stealing your central vision. It doesn’t take your sight entirely, but it takes the part you rely on most: reading, driving, recognizing faces. And for millions of people over 55, it’s the leading cause of vision loss in developed countries.
AMD comes in two forms: dry and wet. About 9 out of 10 cases are dry AMD. It starts slowly, with tiny yellow deposits called drusen building up under the retina. Over years, the macula - the central part of the retina responsible for sharp, detailed vision - begins to thin and break down. This is called geographic atrophy. You might notice things getting dimmer, colors less vibrant, or text becoming harder to read. But it’s the wet form that changes everything fast.
Wet AMD affects only 10-15% of people with AMD, yet it causes 90% of the severe vision loss. It happens when abnormal blood vessels grow under the macula. These vessels leak fluid and blood, scarring the retina in weeks or months. Without treatment, central vision can drop from 20/40 to 20/200 - legally blind - in less than a year. That’s why catching wet AMD early is critical.
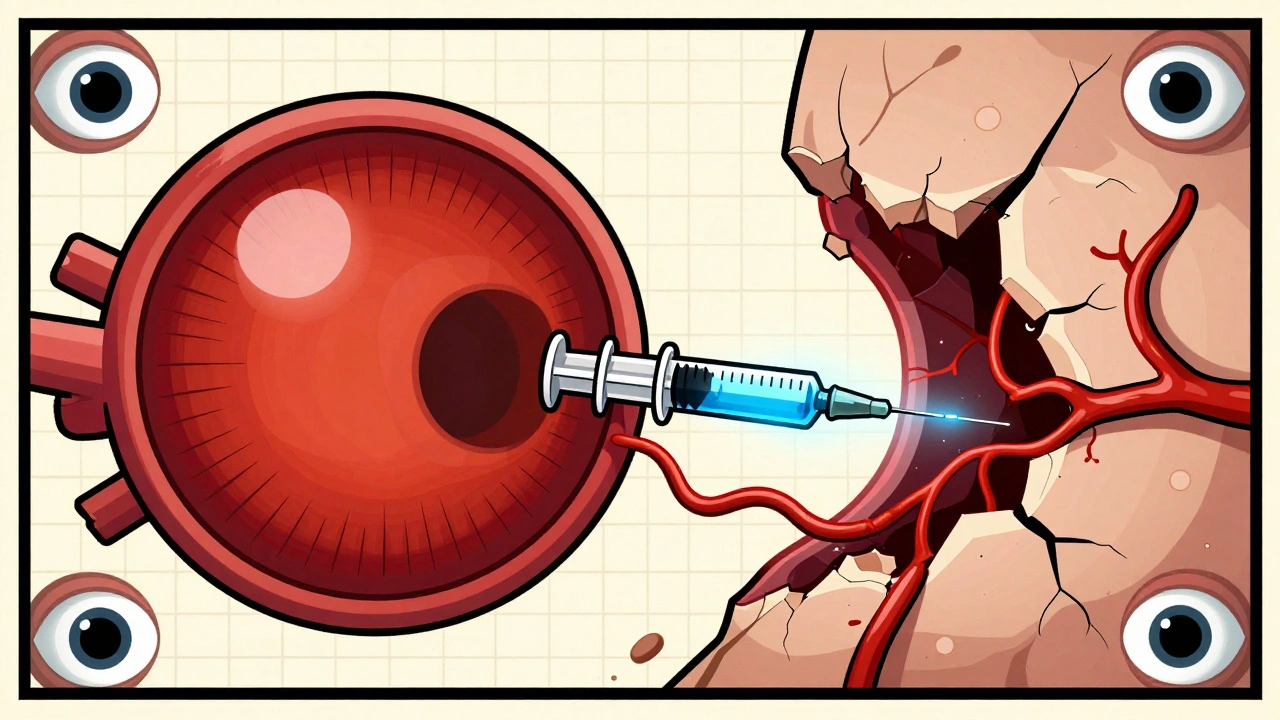
The good news? We have a powerful tool to stop it: anti-VEGF therapy. VEGF stands for vascular endothelial growth factor. It’s a protein your body makes to help grow blood vessels - useful when you’re healing a cut, but dangerous when it’s spurring abnormal vessels in your eye. Anti-VEGF drugs block that signal. They’re injected directly into the eye, usually every 4 to 8 weeks at first. These aren’t pills or eye drops. They’re tiny needles, administered in a clinic, under local numbing drops. It sounds scary, but most patients say the discomfort is brief and manageable.
Studies show that 68% of people who start anti-VEGF treatment stabilize or even improve their vision. One patient in Melbourne, 72, had vision drop to 20/200 after a sudden blur. After 12 injections over nine months, it improved to 20/40. He still drives, still reads the newspaper. He calls it the best decision he ever made, even though he hates the clinic visits.
But the treatment isn’t perfect. The biggest complaint? The frequency. Monthly or bi-monthly shots for months on end. Some people miss appointments because of transportation, fear, or fatigue. And missing even one injection can cost you vision. Research shows patients who skip more than 25% of their scheduled shots lose 30% more vision than those who stick to the plan.
That’s why new options are coming. In 2021, the FDA approved Susvimo - a tiny implant placed in the eye that slowly releases ranibizumab for up to six months. It cuts injection visits from 12 a year to just two. Then in 2022, Vabysmo hit the market - a single drug that blocks two targets: VEGF and another protein called angiopoietin-2. Early results suggest it may work longer between doses. These aren’t cures, but they’re steps toward less burden and better outcomes.
Anti-VEGF isn’t the only piece of the puzzle. Nutrition matters. The AREDS2 formula - a specific mix of vitamins C, E, zinc, copper, lutein, and zeaxanthin - reduces the risk of dry AMD progressing to the wet form by 25%. It’s not a miracle cure, but for someone with intermediate AMD, it’s one of the few proven ways to slow things down. And if you smoke? Quitting cuts your risk of developing wet AMD by more than half. Smoking isn’t just bad for your lungs - it’s a direct accelerator for macular degeneration.
Genetics play a role too. If a parent or sibling has AMD, your risk triples to six times higher. And while it’s more common in White populations, it affects everyone. Age is the biggest risk factor. Less than 1% of people under 50 have AMD. By age 75, that jumps to 35%. That’s why annual eye exams after 65 aren’t optional - they’re essential. Ophthalmologists use optical coherence tomography (OCT), a non-invasive scan, to see layers of the retina in detail. It can catch fluid buildup before you even notice vision changes.
At home, you can monitor yourself with the Amsler grid - a simple chart with straight lines and a dot in the center. If the lines look wavy, broken, or blurry in the middle, it could mean wet AMD is developing. About 40% of patients catch early signs this way before their next appointment. It’s free, it’s quick, and it could save your vision.
The cost of AMD is staggering. In the U.S. alone, it costs $4.6 billion a year in medical care. Globally, the anti-VEGF market was worth over $8 billion in 2022. Drugs like Lucentis, Eylea, and Beovu dominate, but newer treatments are slowly shifting the landscape. Ophthalmologists now use anti-VEGF as first-line treatment in 92% of wet AMD cases - up from just 15% in 2005. That’s a revolution in 20 years.
There’s hope on the horizon. Gene therapy trials are targeting the complement system - a part of the immune system that’s overactive in about 70% of AMD cases. Early results suggest it might one day prevent the disease before it starts. For now, though, the best defense is early detection, consistent treatment, and lifestyle changes.
You can’t reverse AMD. But you can stop it from stealing your life. Whether it’s sticking to your injection schedule, taking your AREDS2 vitamins, quitting smoking, or checking the Amsler grid every week - these small actions add up. Vision loss isn’t inevitable. With the right care, many people keep reading, driving, and seeing their grandchildren’s faces for years longer than they thought possible.
What are the main types of age-related macular degeneration?
There are two main types: dry and wet. Dry AMD is the most common - about 90% of cases. It’s caused by drusen, which are fatty protein deposits under the retina. Over time, these lead to thinning of the macula, a process called geographic atrophy. Vision loss is slow, often over years.
Wet AMD is less common but far more aggressive. It happens when abnormal blood vessels grow under the macula, leaking fluid and blood. This damages photoreceptor cells quickly. Wet AMD always counts as late-stage disease, and it’s responsible for most severe vision loss from AMD.
How does anti-VEGF therapy work?
Anti-VEGF therapy blocks a protein called vascular endothelial growth factor, which triggers the growth of abnormal blood vessels in the eye. In wet AMD, these vessels leak and scar the retina. Anti-VEGF drugs - injected directly into the eye - stop that process. They don’t cure AMD, but they can stop vision from getting worse and sometimes even improve it.
How often do you need anti-VEGF injections?
Typically, patients get injections every 4 weeks for the first 3 months. After that, treatment switches to an as-needed schedule based on eye scans (OCT). Some people need shots every 6 to 8 weeks. Newer treatments like Vabysmo and the Susvimo implant aim to extend the time between injections to 3-6 months.
Can you prevent AMD?
You can’t prevent it entirely, but you can lower your risk. Don’t smoke. Eat leafy greens and fish rich in omega-3s. Take the AREDS2 supplement if you have intermediate AMD. Control blood pressure and cholesterol. Wear UV-blocking sunglasses. And get annual eye exams after age 65.
Does AMD cause total blindness?
No. AMD affects only central vision. Peripheral vision - what you see out of the corners of your eyes - usually stays intact. That means you can still navigate a room, move around, and see large objects. But tasks requiring detail - reading, driving, recognizing faces - become very difficult without central vision.
What happens if you miss an anti-VEGF injection?
Missteps matter. Studies show patients who miss more than 25% of their scheduled injections lose 30% more vision than those who stay on track. Even one missed shot can allow fluid to build up again, causing new damage. Consistency is key to preserving vision long-term.







John Filby
December 5, 2025 AT 06:59Elizabeth Crutchfield
December 6, 2025 AT 17:51Isabelle Bujold
December 7, 2025 AT 20:35Ashley Elliott
December 8, 2025 AT 10:29Joe Lam
December 9, 2025 AT 21:34Chase Brittingham
December 11, 2025 AT 09:43Bill Wolfe
December 12, 2025 AT 16:40Augusta Barlow
December 14, 2025 AT 03:57michael booth
December 15, 2025 AT 12:42Alex Piddington
December 16, 2025 AT 04:16Chad Handy
December 16, 2025 AT 09:40