When you pick up a prescription, you might not notice the difference between the brand-name pill and the generic version sitting in your hand. Same shape, same color, same label - but a fraction of the price. That’s therapeutic equivalence at work. It’s not just a regulatory buzzword. It’s the scientific guarantee that your generic medication will do exactly what the brand-name version does - without putting your health at risk.
What Therapeutic Equivalence Actually Means
Therapeutic equivalence means two drugs - one brand-name, one generic - contain the same active ingredient, in the same amount, delivered the same way, and will produce the same effect in your body. The U.S. Food and Drug Administration (FDA) uses this standard to approve generic drugs. It’s not enough for a generic to have the same chemical on the label. It must behave the same inside you. The FDA’s Orange Book, updated every October, is the official list of all approved drugs and their therapeutic equivalence ratings. As of October 2023, it includes over 13,000 drug products. Each one gets a two-letter code. If you see an "A" - like AB, AC, or AO - that drug is rated as therapeutically equivalent to its brand-name counterpart. That means you can safely switch without worrying about your treatment failing or your side effects changing.The Three Rules Behind the Rating
Getting that "A" rating isn’t easy. It requires passing three strict tests:- Pharmaceutical equivalence: The generic must have the exact same active ingredient, strength, dosage form (tablet, capsule, injection), and route of administration (oral, topical, etc.) as the brand. Inactive ingredients like fillers or dyes can be different - but they can’t affect how the drug works.
- Bioequivalence: This is where the science gets real. The generic must be absorbed into your bloodstream at the same rate and to the same extent as the brand. The FDA requires that the 90% confidence interval for the ratio of key measurements - AUC (total exposure) and Cmax (peak concentration) - falls between 80% and 125%. In plain terms: your body gets within 20% of the same dose as the brand. For most drugs, that’s safe.
- Identical clinical effect: The drug must work the same way in real patients. This isn’t just about blood levels. It’s about whether your blood pressure drops, your cholesterol goes down, or your seizure frequency stays controlled. If it doesn’t, it doesn’t get an "A" rating.
Why This Matters for Patient Safety
Imagine you’re on warfarin, a blood thinner with a very narrow window between too little and too much. A 5% change in absorption could mean a clot or a bleed. For drugs like this, the FDA doesn’t use the standard 80-125% range. It demands tighter control: 90-110%. That’s because therapeutic equivalence isn’t one-size-fits-all. It adapts to risk. The system works. A 2022 UnitedHealthcare survey of 12,500 patients who switched to generic drugs rated as therapeutically equivalent found 87% reported no change in how they felt. Only 3.2% blamed the switch for any side effects. And when the Institute for Safe Medication Practices looked at 127 reported adverse events tied to generic substitution between 2018 and 2022, only 17 involved drugs with an "A" rating. Most were due to patient anxiety, mislabeling, or switching to a product that wasn’t even rated equivalent.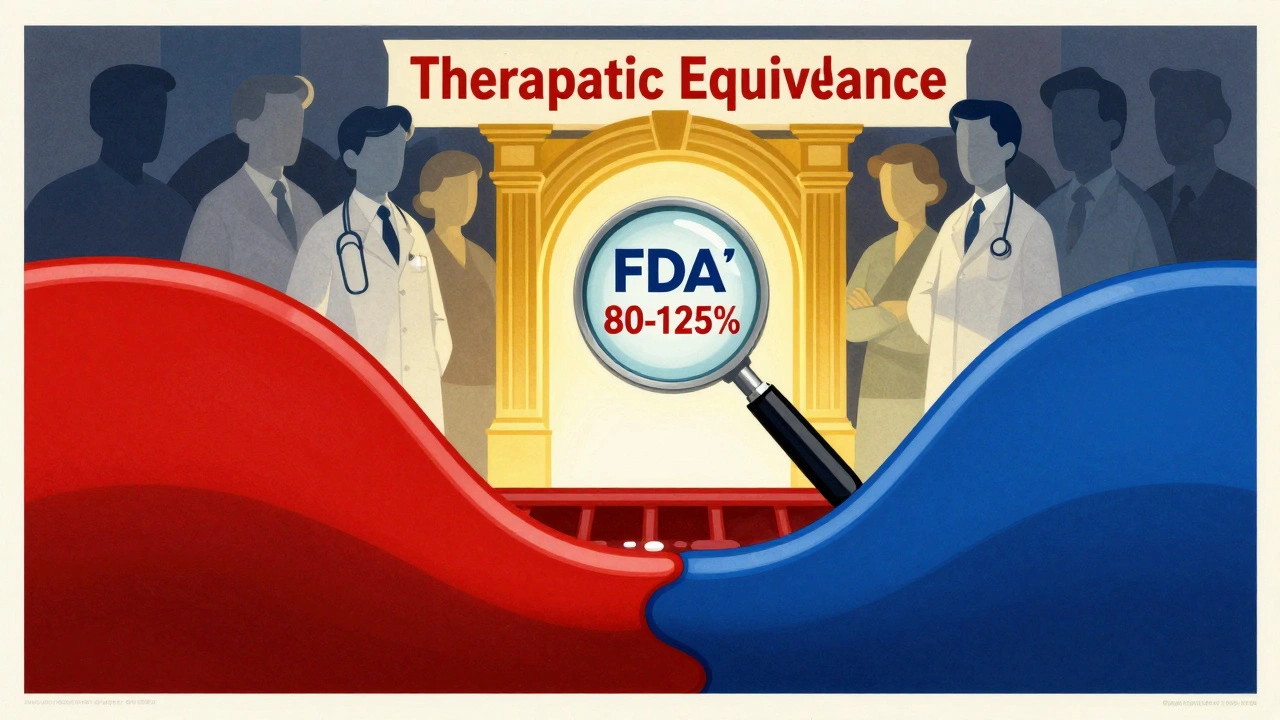
What Happens When It Doesn’t Work?
Not all generic drugs are created equal - and not all substitutions are safe. Some products get a "B" rating. That means the FDA has found evidence that they might not be therapeutically equivalent. These include certain extended-release formulations, complex inhalers, or topical creams where traditional blood tests can’t reliably predict performance. Pharmacists aren’t allowed to substitute these without a doctor’s approval. There’s also therapeutic interchange - swapping one drug for another in the same class, like switching from one statin to another. But that’s not therapeutic equivalence. A 2019 JAMA Internal Medicine study showed that therapeutic interchange led to 32% more adverse events than switching between therapeutically equivalent generics. Why? Because different drugs have different side effect profiles, even if they treat the same condition.How Pharmacists Use the Orange Book
Your pharmacist checks the Orange Book every time you fill a prescription. In 49 U.S. states, they can automatically substitute a generic if it’s rated "A" - no need to call your doctor. But in 11 states, the prescriber must write "Dispense as Written" on the prescription to block substitution. Understanding the two-letter codes matters. The first letter tells you if the drugs are equivalent (A = yes, B = no). The second letter adds detail - like whether it’s an immediate-release tablet (B), an extended-release capsule (C), or a product with special considerations (O). Pharmacists get training on this. The FDA offers free 90-minute online modules. After completing them, 85% of participants improved their accuracy in identifying equivalent products.
The Bigger Picture: Cost, Access, and Trust
Generic drugs make up 90.7% of all prescriptions filled in the U.S. - but they account for only 58% of total drug spending. That’s $158 billion saved every year because of therapeutic equivalence. Without it, millions of people couldn’t afford their medications. And yet, trust remains an issue. Some patients report feeling worse after switching - even when the drug is rated "A." Often, it’s not the drug. It’s the fear. A change in pill color or size can trigger anxiety. Some people confuse therapeutic equivalence with therapeutic interchange. Others hear stories online - like Reddit threads where people blame generics for side effects - without realizing many of those cases involved "B"-rated products or non-equivalent switches. The FDA and medical groups like the American Medical Association have repeatedly affirmed: therapeutically equivalent generics are safe. Dr. Janet Woodcock, former head of the FDA’s drug center, said in 2021: "The FDA’s therapeutic equivalence determinations provide assurance that generic drugs perform the same way as brand name drugs in the body."What’s Next for Therapeutic Equivalence?
The system isn’t perfect. Complex drugs - like inhalers, injectables, or topical creams - are harder to test. Traditional blood-level measurements don’t always reflect how well the drug works in the lungs or skin. In November 2023, the FDA released draft guidance for evaluating these products, using new methods like imaging and real-world data. The agency is also investing $65 million through 2027 to improve testing for complex generics under GDUFA III. And in a partnership with MIT, the FDA is testing artificial intelligence to predict which formulation changes might break therapeutic equivalence before a drug even hits the market. Meanwhile, the number of generic approvals keeps rising. In 2022 alone, the FDA approved 1,257 new generics - all of them required to meet the same high bar.What You Should Do
If you’re prescribed a generic drug:- Ask your pharmacist if it’s rated "A" in the FDA Orange Book. If it is, you’re safe.
- Don’t assume all generics are the same. If you’ve had issues before, ask for the brand or check the rating.
- Report any new or worsening side effects - even if you think it’s "just the pill looking different."
- Don’t switch between generics unless your doctor or pharmacist says it’s okay. Even two "A"-rated generics aren’t always interchangeable if they’re different formulations.







Allan maniero
December 2, 2025 AT 06:29Man, I’ve been on generics for years-blood pressure med, cholesterol, you name it. Never had a hiccup. I used to be paranoid too, thought the little blue pill was gonna turn into a green one and I’d start seeing things. Turns out, my body doesn’t care what the label says, just what’s in it. The FDA’s got this locked down tighter than my ex’s Instagram privacy settings. Seriously, if you’re not on generics, you’re just paying for marketing and fancy packaging. My pharmacist even showed me the Orange Book once. It’s like the Yelp of pharmaceuticals, but way less spammy.
Anthony Breakspear
December 3, 2025 AT 22:50Bro, therapeutic equivalence is the unsung hero of American healthcare. No cap. We’re talking about saving $158 billion a year so grandma can afford her blood thinner without choosing between pills and peanut butter. And yeah, some folks freak out when the pill looks different-color, shape, whatever. But that’s not the drug’s fault, that’s your brain playing tricks on you. I had a buddy swear his generic Adderall made him ‘zombie-like’ until we checked the Orange Book-turns out he got switched to a B-rated version. Classic. The system works. Trust the science, not the Reddit memes.
Saket Modi
December 4, 2025 AT 16:56generic = bad lol
Chris Wallace
December 5, 2025 AT 23:05I’ve been a nurse for 18 years, and I’ve seen patients panic over generic switches more than actual side effects. The fear isn’t irrational-it’s cultural. We’ve been sold the idea that brand-name = better, even when the science says otherwise. I always sit down with patients, show them the Orange Book code, explain what bioequivalence actually means in plain terms. Most of them relax after five minutes. The real issue isn’t the drugs-it’s the lack of education. If we taught this in high school biology, we’d cut down on so much unnecessary anxiety. And honestly? The FDA’s doing better than most industries at keeping things transparent.
william tao
December 6, 2025 AT 09:18While it is undeniably laudable that the Food and Drug Administration has instituted a rigorous framework for assessing therapeutic equivalence, one cannot help but observe the alarming epistemological fragility of relying on statistical confidence intervals-specifically the 80-125% range-as a proxy for clinical equivalence. This is not pharmacology; it is probabilistic approximation masquerading as certainty. Moreover, the implicit assumption that pharmacokinetic parameters (AUC and Cmax) are sufficient to predict pharmacodynamic outcomes is, in my view, a gross oversimplification of human physiology. The Orange Book, while useful, is a bureaucratic artifact-not a theological scripture. One must question whether the cost savings justify the potential for subclinical, long-term deviations in therapeutic outcomes, particularly in vulnerable populations.
Sheryl Lynn
December 7, 2025 AT 12:28Ugh, I just had to switch from my $200/month brand-name antidepressant to a generic because my insurance ‘decided’ to ‘save me money.’ And guess what? I felt like a zombie for three weeks. It wasn’t my fault-I followed the script. But now I’m stuck in this limbo where my psychiatrist says ‘it’s the same,’ but my soul says otherwise. And don’t even get me started on the pill color change. It was lavender before, now it’s beige. Beige?! That’s not medicine, that’s a sad IKEA shelf. I don’t care what the Orange Book says-I’m paying extra next time. My mental health isn’t a cost-cutting experiment.
Paul Santos
December 7, 2025 AT 13:14Therapeutic equivalence? More like therapeutic *illusion*, amirite? 😏 We’re talking about drugs that are ‘bioequivalent’ within 20%-so your body could be getting 80% of the dose, or 125% of it. That’s not precision, that’s a dartboard with blindfolded toddlers throwing darts. And don’t get me started on the ‘A’ rating. It’s like saying two different brands of soy sauce are ‘equivalent’ because they’re both salty. They’re not. One’s got umami, the other’s got regret. I’ve seen people crash after switching. The FDA’s not wrong-they’re just… optimistic. And honestly? I’m not paying for the placebo of ‘trust.’ I’m paying for peace of mind. 🤷♂️
Eddy Kimani
December 8, 2025 AT 22:29Interesting how the FDA’s 80-125% bioequivalence window was derived from population-level PK/PD modeling, but individual variability-especially in CYP450 metabolizers-can push someone outside that range. I’ve seen case reports where patients with poor CYP2D6 activity had therapeutic failure with generics for SSRIs, even when rated ‘A.’ The system’s robust, but not infallible. The real gap is in pharmacogenomic integration-nobody’s mapping genetic profiles to generic substitution yet. Maybe that’s the next frontier? Could AI predict who’s at risk before the switch? 🤔
Chelsea Moore
December 10, 2025 AT 19:26AND YET-people still die from generic substitutions! Did you read about the 82-year-old woman in Ohio who had a stroke after switching to a generic warfarin? The FDA says ‘it’s safe’-but what about the 3.2%? What about her?!! She didn’t sign up for a lottery! This isn’t science-it’s corporate greed wrapped in a lab coat! And now they’re pushing AI to ‘predict’ equivalence?! That’s like letting a toddler drive a tank because ‘it’s probably fine!’ I’m done. I’m switching back to brand. My life is worth more than $50 a month.
John Biesecker
December 12, 2025 AT 14:02you know what’s wild? i used to think generics were just ‘cheap copies’… then my dad got on one for his diabetes med and his A1c dropped. like, actually dropped. i was like… huh. maybe the science isn’t just for show? 🤯 also, the orange book is kinda like a drug version of ‘this or that’ but with way more paperwork. and honestly? i trust it more than my ex’s text messages. 🤓
Genesis Rubi
December 13, 2025 AT 20:46Generic drugs? In AMERICA? Please. We’re the most advanced country on Earth and we’re letting some lab in India make our meds? My grandpa used to say ‘you get what you pay for.’ And I pay for AMERICAN quality. The FDA’s just playing politics. They approve generics to save money for Big Pharma’s shareholders. Meanwhile, real Americans are getting sick from ‘equivalent’ pills made overseas. This isn’t innovation-it’s surrender. And if you’re okay with this, you’re not patriotic. You’re just lazy.
Anthony Breakspear
December 14, 2025 AT 11:56Sheryl Lynn, I feel you. I had the same thing happen with my anxiety med-pill turned from white to yellow, I started sweating at night like I’d been sprinting through a sauna. Turns out, it was the filler. Not the active ingredient. But the FDA didn’t care because the bioequivalence numbers were fine. So I asked my doc to write ‘Dispense as Written’ and paid the extra $15. My peace of mind? Priceless. And no, I’m not ‘anti-generic’-I’m pro-not-getting-sick-from-a-pill-that-looks-like-a-throw-up-bag.