Opioid Nausea Risk Calculator
Opioid Selection
Nausea Symptoms
Nausea Risk Assessment
Nausea Risk Level
Select an opioid to view its nausea risk profile.
Recommended Antiemetic
Select symptoms to view appropriate antiemetic recommendations.
When opioids are prescribed for pain, nausea and vomiting often come along for the ride. It’s not rare. About one in three patients on opioids will feel sick to their stomach. For many, this isn’t just an inconvenience-it’s the reason they stop taking their pain medication altogether. A study from Smith in 2012 found that patients would rather live with more pain than deal with nausea. That’s how powerful this side effect is. But here’s the catch: giving antiemetics before nausea even starts doesn’t always help. And mixing the wrong drugs can be dangerous.
Why Opioids Make You Nauseous
Opioids don’t just dull pain-they mess with your brain and gut in several ways at once. The main culprit is how they activate opioid receptors in the brainstem, especially in an area called the chemoreceptor trigger zone. This zone normally detects toxins and triggers vomiting. Opioids trick it into thinking there’s poison, even when there isn’t.
Another mechanism? Slowed digestion. Opioids tighten up the muscles in your stomach and intestines. Food sits longer. Gas builds up. That pressure can trigger nausea. And if you’re sensitive to motion-like turning your head or standing up-you might feel dizzy or queasy because opioids also affect your inner ear balance system.
It’s not one problem. It’s three: brain chemistry, gut slowdown, and balance disruption. That’s why some antiemetics work for some people but not others.
Which Antiemetics Actually Work?
There are three main classes of antiemetics used for opioid-induced nausea, and each targets a different pathway.
- 5-HT3 antagonists (ondansetron, palonosetron): Block serotonin in the gut and brain. These are often the first choice. A study by Moon and colleagues showed palonosetron cut nausea rates from 62% to 42% compared to ondansetron.
- Dopamine antagonists (metoclopramide, droperidol): Block dopamine receptors in the brain’s vomiting center. But here’s the twist: a Cochrane review by Gottlieb in 2022 found that giving metoclopramide before an opioid didn’t reduce nausea at all in three small trials.
- Anticholinergics and antihistamines (scopolamine, meclizine): These help when nausea comes from dizziness or movement. Useful if patients feel sick when they stand up or turn their head.
But not all antiemetics are safe. Both droperidol and ondansetron carry FDA black box warnings. Why? They can lengthen the QT interval on an ECG, raising the risk of dangerous heart rhythms. This isn’t theoretical-it’s real. Patients with heart conditions, older adults, or those on other QT-prolonging drugs (like certain antibiotics or antidepressants) are at higher risk.
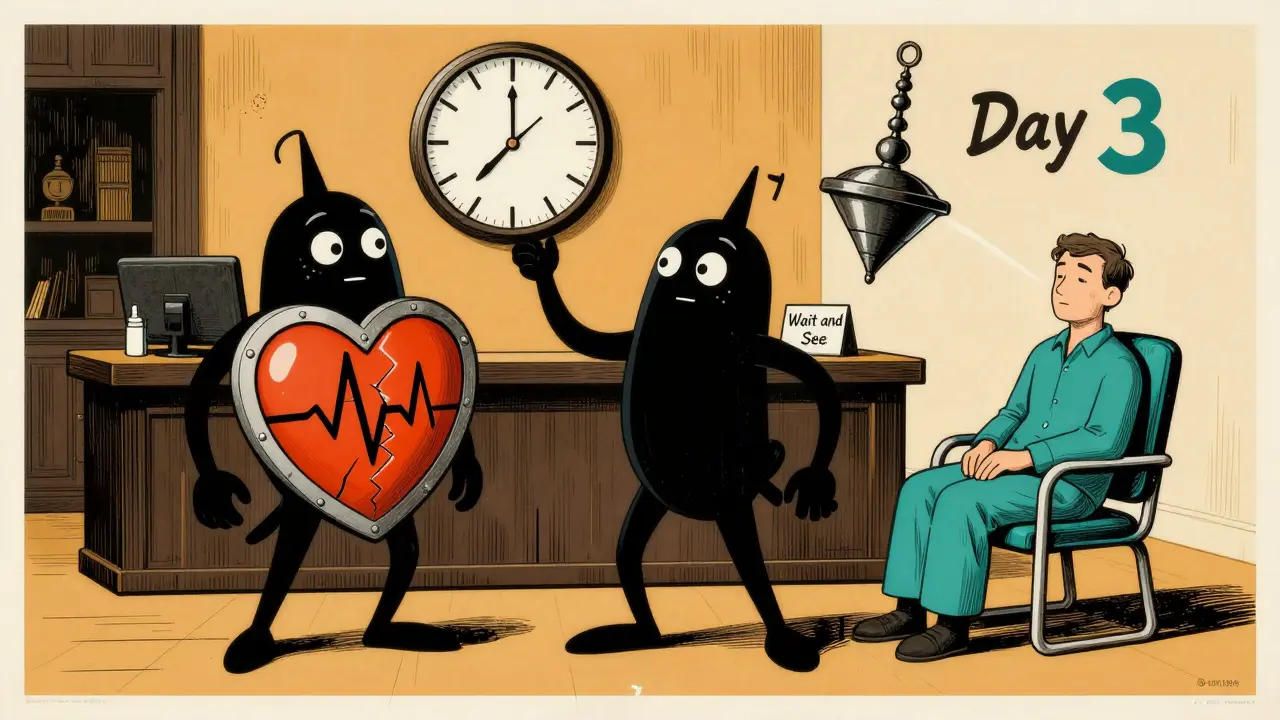
Prophylaxis vs. Reactive Treatment
Should you give antiemetics before nausea starts? Or wait until it happens?
The evidence leans toward waiting. The Cochrane review found no benefit to giving metoclopramide before intravenous opioids. That’s surprising, because it’s been done for decades. But newer data shows most patients don’t need it. Why? Because tolerance builds fast.
Most people who get nausea on a new opioid will feel better in 3 to 7 days-without any antiemetic at all. That’s the natural history of opioid-induced nausea. So, instead of giving a drug to everyone, a smarter approach is to wait. If nausea hits, treat it. If it goes away on its own, you avoided unnecessary side effects and drug interactions.
There’s one exception: patients who’ve had severe nausea before, or those with high sensitivity to motion. For them, a short course of an antiemetic in the first few days might make a difference.
Drug Interactions You Can’t Afford to Miss
Combining opioids with antiemetics isn’t the only risk. Mixing opioids with other drugs can be deadly.
The FDA has warned that opioids can interact with antidepressants (like SSRIs and SNRIs), migraine medications (triptans), and even some antibiotics. Together, they can trigger serotonin syndrome-a rare but life-threatening condition. Symptoms? Agitation, fast heart rate, high temperature, muscle rigidity. It can escalate in hours.
Also, combining opioids with benzodiazepines or sleep aids slows breathing even more. That’s why the CDC’s 2022 guideline says doctors must warn patients about all these risks before prescribing opioids. It’s not just about nausea. It’s about breathing.
And don’t forget: some antiemetics themselves slow breathing. Droperidol, for example, has been linked to respiratory depression in older patients. So you’re treating nausea but risking something worse.
Best Practices: What Actually Works
There’s no one-size-fits-all solution. But here’s what the evidence and guidelines agree on:
- Start low, go slow. A low opioid dose at first reduces side effects. For example, morphine at 1 mg twice daily for chronic breathlessness causes far less nausea than 10 mg. Slow titration gives the body time to adjust.
- Rotate opioids. Not all opioids cause the same nausea. Tapentadol causes about 3-4 times less nausea than oxycodone per dose. Oxymorphone? About 60 times worse. Switching opioids can cut nausea without losing pain control.
- Don’t pre-treat unless needed. Don’t give antiemetics to everyone. Only give them if nausea develops. Then pick the right one based on symptoms-dizziness? Try scopolamine. Gut-based nausea? Try palonosetron.
- Review all medications. Check for interactions with antidepressants, antibiotics, heart meds, and other CNS depressants. Use tools like drug interaction checkers in your EHR.
- Educate patients. Tell them upfront: “You might feel nauseous in the first few days. It usually passes. Don’t stop your pain medicine unless you’re having trouble breathing.” That simple message improves adherence.

When to Avoid Antiemetics Altogether
Some patients shouldn’t get antiemetics at all.
If someone has kidney disease, metoclopramide can build up and cause movement disorders. If they’re on other QT-prolonging drugs, ondansetron or droperidol could trigger arrhythmias. If they’re elderly, anticholinergics like scopolamine can cause confusion or urinary retention.
And here’s the hard truth: many antiemetics are overused. Clinicians give them out of habit, not evidence. But the data doesn’t support blanket use. It supports thoughtful, individualized care.
The Bottom Line
Opioid-induced nausea is common-but not inevitable. It’s not a reason to avoid opioids. It’s a reason to use them smarter.
Don’t give antiemetics just because you can. Don’t assume all nausea is the same. Don’t ignore drug interactions. And don’t forget: most nausea fades on its own in a week.
The best strategy? Start low, watch closely, treat only if needed, and always check what else the patient is taking. That’s how you keep pain under control-and keep people safe.
Do all opioids cause nausea equally?
No. Opioids vary widely in how much nausea they cause. Oxymorphone has the highest risk-about 60 times more nausea per dose than oxycodone. Tapentadol causes far less nausea than oxycodone, around 3-4 times lower. Morphine and hydromorphone fall in the middle. Choosing a lower-emetic opioid can reduce nausea without changing pain control.
Should I give ondansetron before an opioid dose?
Not routinely. Studies show no benefit to giving ondansetron or metoclopramide before opioid administration. The Cochrane review found no reduction in nausea or vomiting. Instead, wait to see if nausea develops. If it does, treat it with a 5-HT3 antagonist like palonosetron or ondansetron-but only if the patient doesn’t have heart risks.
Can antiemetics make opioid side effects worse?
Yes. Some antiemetics, like droperidol and metoclopramide, can slow breathing, especially in older adults or those with lung disease. Others, like anticholinergics, can cause confusion or urinary retention. Even ondansetron carries a risk of dangerous heart rhythms. So using them without need increases risk without benefit.
How long does opioid-induced nausea last?
For most people, nausea fades within 3 to 7 days as the body develops tolerance to the drug. This is why prophylactic antiemetics are often unnecessary. If the patient is stable on a fixed dose, the nausea will usually resolve on its own without intervention.
Is serotonin syndrome a real risk with opioids and antiemetics?
Yes. Opioids can interact with antidepressants (SSRIs, SNRIs), migraine drugs (triptans), and even some antiemetics like metoclopramide to trigger serotonin syndrome. Symptoms include agitation, high fever, fast heartbeat, and muscle stiffness. It’s rare but life-threatening. Always check for these combinations before prescribing.





