There’s a lot of confusion out there about affirmative consent and how it relates to medical care. Some people think it means doctors need a patient to say "yes" out loud every time they change a treatment plan. Others believe it’s the same rule used in sexual assault policies - and that’s where things go off track. The truth? Affirmative consent laws don’t apply to medical substitution at all. They were never meant to. Mixing these two systems creates real problems - delays in care, misunderstandings between patients and providers, and even legal risks for hospitals.
What Affirmative Consent Actually Is
Affirmative consent laws started appearing in U.S. states around 2014, mostly on college campuses. California’s Senate Bill 967 was one of the first. It said that for sexual activity to be legal, both people must give affirmative, conscious, and voluntary agreement - not just the absence of a "no." This became known as the "yes means yes" standard. It’s about active communication, ongoing permission, and the ability to withdraw consent at any moment.
These laws were created to address sexual violence. They apply to relationships, parties, dorm rooms, and campus policies. They don’t mention hospitals, surgeries, or prescriptions. And they don’t apply when someone is unconscious, intoxicated, or mentally incapacitated - because under these laws, that person cannot give consent at all.
How Medical Consent Actually Works
When a patient walks into a doctor’s office, the legal standard isn’t "yes means yes." It’s informed consent. That means the provider explains:
- What the condition is
- What the treatment does
- What the risks and benefits are
- What other options exist
- What happens if they do nothing
- Whether they’re capable of understanding this information
Then the patient says "yes" - verbally, by signing a form, or by just showing up for the procedure. No ongoing check-ins. No need to reconfirm every five minutes. This system has been around since the 1914 Schloendorff v. Society of New York Hospital case, and it’s been refined through decades of court rulings and state laws.
California’s Civil Code Section 56.11, for example, requires doctors to disclose "all material risks" before treatment. That’s it. No "enthusiastic" approval needed. No "ongoing" affirmation. Just clear communication and voluntary agreement.
What Happens When a Patient Can’t Consent?
Now imagine a patient is in a coma after a car crash. They can’t say "yes" or "no." What happens then?
This is where substituted judgment kicks in - not affirmative consent. The law doesn’t ask a family member to say "yes" loudly and clearly. It asks them: "What would this patient have chosen, if they could speak?"
Doctors look to:
- Advance directives (like living wills)
- Previously expressed wishes ("I don’t want to be kept alive on machines")
- Religious beliefs or cultural values the patient held
- Decisions made by a legally appointed healthcare proxy
California Health and Safety Code Section 7185 says surrogates must use substituted judgment - not what they personally think is best. If there’s no advance directive, then the decision shifts to "best interest" - meaning what a reasonable person would choose under similar circumstances.
This is a completely different system than "yes means yes." It’s not about loud agreement. It’s about quiet, thoughtful decision-making based on known values.

Why People Get Confused
It’s not hard to see why this mix-up happens. Both involve the word "consent." Both deal with autonomy. Both are about rights. But they operate in totally different worlds.
At the University of Colorado Denver, a 2023 survey found 78% of undergraduates couldn’t tell the difference between medical consent and sexual consent standards. That’s not surprising. Campuses run training on affirmative consent. Hospitals don’t. Students hear "consent" in both places and assume it’s the same rule.
Even some medical students get tangled up. On Reddit’s r/medschool, a top comment from January 2023 said: "Affirmative consent is for sexual activity policies on campus; medical consent uses different standards based on patient capacity and disclosure requirements." That comment got over 1,200 upvotes. Why? Because it’s true.
The confusion isn’t just academic. In 2023, a hospital in Oregon nearly delayed emergency surgery because a nurse insisted the patient’s daughter "say yes out loud" - thinking affirmative consent applied. The patient was sedated and couldn’t respond. The doctor had to pull out the advance directive to explain why the daughter’s prior statements were legally sufficient. No verbal affirmation needed.
What Happens If You Apply Affirmative Consent to Medicine?
Let’s say you tried to force "yes means yes" into a hospital setting. What would happen?
- A patient in pain after surgery needs a new IV. The nurse asks, "Do you want this?" The patient moans. Is that "affirmative" enough? What if they’re too drowsy to speak?
- A child with pneumonia needs antibiotics. The parent says "yes," but doesn’t smile. Is that "enthusiastic"? What if they’re stressed and exhausted?
- An elderly patient with dementia has a living will that says "no CPR." The doctor asks the son: "Do you agree with this?" The son says "yes," but looks unsure. Do you wait for him to say it louder?
These aren’t hypotheticals. They’re real situations doctors face every day. If you applied sexual consent standards to medicine, you’d slow down emergencies, confuse families, and create legal gray zones where none should exist.
The Federation of State Medical Boards put it plainly in March 2023: "Applying sexual consent standards to medical decision-making creates unnecessary barriers to urgent care and misunderstands the legal foundations of medical consent."
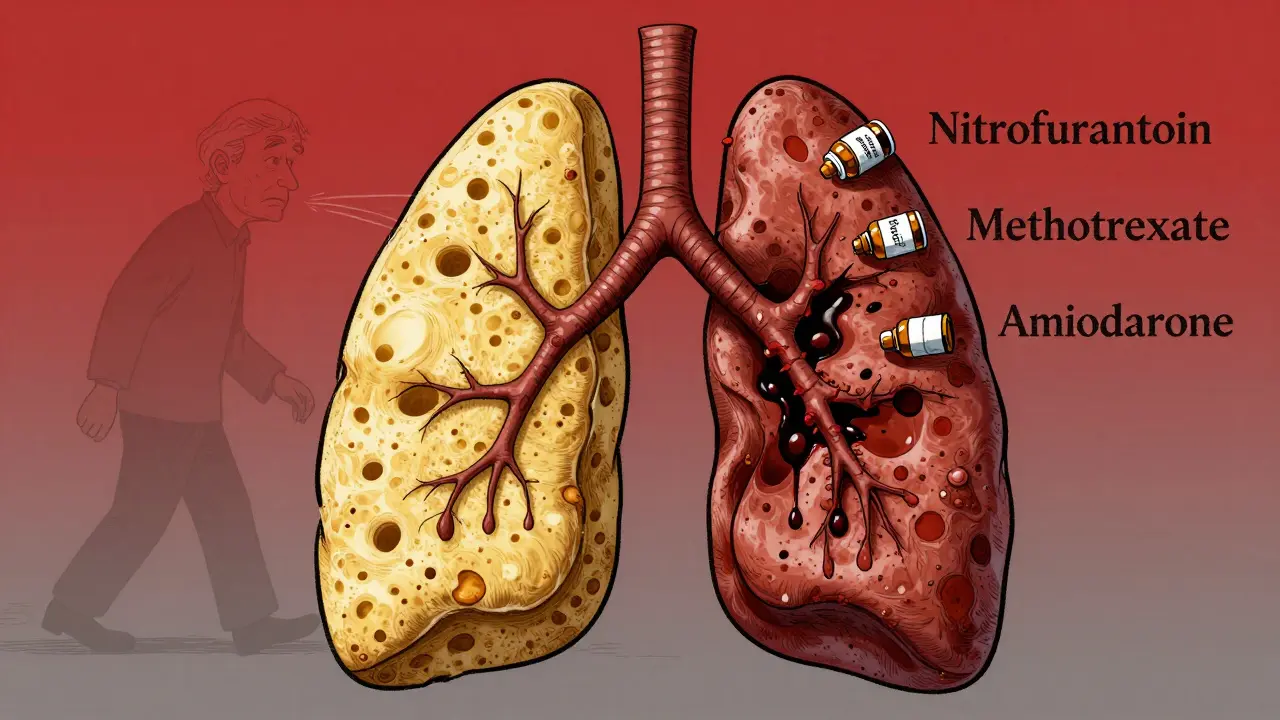
![]()
What’s the Right Way Forward?
Clear separation is the only solution. Here’s what works:
- For sexual activity: Use affirmative consent - ongoing, verbal, enthusiastic, reversible.
- For medical care: Use informed consent - clear explanation, understanding, voluntary agreement.
- For incapacitated patients: Use substituted judgment or best interest - based on known values, not new affirmations.
Hospitals and universities need to train staff separately. Medical students should learn about advance directives and surrogate decision-making. Campus safety teams should focus on boundaries, intoxication, and power dynamics - not medical forms.
California’s 2022 AB569 law made this clear: it updated sexual consent rules - and left medical consent untouched. The federal CARE Act in 2023 focused only on advance directives. No mention of "affirmative." No blending of systems.
Legal scholar Deborah Denno from Fordham Law Review put it best in April 2023: "There is zero likelihood of affirmative consent standards being applied to medical substitution scenarios. The purposes, histories, and practical needs are too different."
What Patients Should Know
If you’re signing a medical form, you’re not being asked to "enthusiastically agree." You’re being asked: "Do you understand what’s going to happen?" If you say yes, that’s enough.
If you’re appointing someone to make decisions for you if you can’t speak, write it down. A living will, a healthcare proxy form - these are your tools. They’re not about loud "yeses." They’re about quiet, thoughtful planning.
And if you ever hear a doctor or nurse say, "We need your family to say yes out loud," ask: "Are you talking about medical consent or sexual consent?" Most of the time, they’ll realize they’ve mixed up the rules - and fix it right away.
Bottom Line
Affirmative consent laws are powerful tools for preventing sexual violence. But they don’t belong in the exam room. Medical consent is built on trust, clarity, and respect - not constant verbal confirmation. Trying to force one into the other doesn’t protect patients. It confuses them.
Understanding the difference isn’t just legal knowledge. It’s patient safety.
Do affirmative consent laws apply to medical procedures?
No. Affirmative consent laws were created for sexual activity and apply only in that context. Medical procedures use informed consent, which requires clear explanation and voluntary agreement - not ongoing verbal affirmation.
What is substituted judgment in medical decision-making?
Substituted judgment is the legal standard used when a patient can’t make their own decisions. The person making the choice (like a family member or proxy) must decide based on what the patient would have wanted, not what they personally think is best. This is guided by advance directives, past statements, or known values.
Can a family member override a patient’s advance directive?
No. An advance directive - like a living will or healthcare power of attorney - is legally binding. Family members can’t override it just because they disagree. Courts and medical teams must follow the patient’s documented wishes unless the document is invalid or outdated.
What if a patient can’t speak but nods their head during treatment?
In medical contexts, non-verbal cues like nodding can count as consent if the patient has the capacity to understand and the action clearly indicates agreement. But this is not the same as affirmative consent in sexual contexts. Medical consent doesn’t require enthusiastic or verbal affirmation - just clear understanding and voluntary action.
Why do people confuse medical consent with affirmative consent?
Both use the word "consent," and both involve personal autonomy. But they’re legally and practically different. Affirmative consent is about active, ongoing permission in sexual situations. Medical consent is about understanding risks and making a choice. The confusion often comes from campus training that doesn’t distinguish between the two.
Is it illegal to perform a procedure without signed consent?
In non-emergency situations, yes. In emergencies where delaying care would cause serious harm, doctors can act without formal consent under the "implied consent" doctrine. But even then, they must document the situation and explain it later. Signing a form isn’t the only way to give consent - understanding and agreement are.
Can minors give consent for medical treatment?
Yes, in specific cases. In California, minors as young as 12 can consent to treatment for STDs, HIV, mental health services, and substance abuse. For other procedures, parental consent is usually required unless the minor is emancipated or in an emergency.




bhushan telavane
December 19, 2025 AT 19:01Man, I read this in India and it made me think - we don’t even have formal consent laws for medical stuff here, just trust and family decisions. But this post? Clear as daylight. No need to overcomplicate.
Alisa Silvia Bila
December 19, 2025 AT 20:21This is exactly why people panic during emergencies.
Alex Curran
December 21, 2025 AT 19:39So many med students think consent is consent is consent until they get burned by a confused nurse or a family member yelling "I didn’t say yes!" in the OR waiting room. The gap between campus training and hospital reality is wild. Honestly, if you’ve never seen a code blue because someone was waiting for a verbal yes, you haven’t worked in ER yet.
Dikshita Mehta
December 22, 2025 AT 14:08It’s funny how language trips us up. "Consent" is one word but carries two completely different legal weights. One is about autonomy in intimacy, the other about autonomy in vulnerability. Mixing them doesn’t empower anyone - it just creates fear. I’ve seen families freeze during ICU meetings because they’re terrified they’ll say the wrong thing. That’s not protection. That’s paralysis.
Dominic Suyo
December 24, 2025 AT 05:39Oh here we go - the medical establishment’s latest crusade against woke culture. Let me guess, next they’ll say "informed consent" is just a fancy way of saying "sign here or we’ll let you die quietly"? Please. You think hospitals don’t weaponize ambiguity? I’ve seen nurses delay meds because the patient "didn’t seem enthusiastic enough." And don’t get me started on the corporate compliance bots who now require 17 forms just to give someone an aspirin. This isn’t clarity - it’s bureaucratic gaslighting dressed up as patient safety.
benchidelle rivera
December 25, 2025 AT 06:16There is no excuse for conflating sexual consent with medical consent. This isn’t semantics - it’s life-or-death confusion. I’ve trained nurses for over a decade and every time someone says "we need affirmative consent for the IV," I have to shut it down immediately. The law doesn’t require enthusiasm. It requires understanding. Period. If you’re teaching students otherwise, you’re not protecting patients - you’re putting them at risk. And if hospitals keep allowing this nonsense, they’ll be sued into oblivion.
Aadil Munshi
December 25, 2025 AT 16:26Let’s be real - the real issue isn’t the law. It’s that people are terrified of being wrong. So they invent rules that don’t exist. "Say it louder!" "Show me you mean it!" - as if a dying man’s nod isn’t enough. We’ve turned healthcare into a performance art where the patient has to audition for their own treatment. And the worst part? The people screaming loudest about "affirmative consent" are the ones who’ve never sat with someone who can’t speak because they’re on a ventilator. You don’t need a yes. You need a memory. A will. A voice they left behind.
Vicki Belcher
December 26, 2025 AT 04:01Thank you for this. 🙏 I’m a nurse and I’ve had families cry because they thought they had to "enthusiastically agree" to a feeding tube. One mom said, "I didn’t smile when I said yes, so I thought I wasn’t allowed." We need to stop making healthcare feel like a dating app. It’s not about vibes - it’s about dignity. And clarity. And honestly? Just… stop overthinking it.
Chris porto
December 27, 2025 AT 17:09There’s something deeply human here. We want to feel like we’re doing right by others. So we invent rules that sound noble - "affirmative consent" - but in practice, they make us more afraid. The real question isn’t whether the law applies - it’s whether we’re treating people like autonomous beings or like potential liabilities. Informed consent isn’t cold. It’s respectful. It says: "I see you. I explained it. You understand. That’s enough." That’s actually more powerful than any shouted yes.
James Stearns
December 28, 2025 AT 06:55Let me be blunt: This is why the public distrusts medicine. You have PhDs writing papers about consent while nurses are told to get a "verbal affirmation" from a sedated patient. Meanwhile, the same institutions that preach "patient autonomy" won’t let a 17-year-old get birth control without parental consent. You want consistency? Then stop pretending your legal frameworks are coherent. They’re not. They’re a patchwork of performative virtue signaling and liability-avoidance masquerading as ethics.
Frank Drewery
December 30, 2025 AT 05:16I’ve sat with patients who couldn’t speak, who looked me in the eye and nodded - and I knew, without a doubt, they were saying yes. No form needed. No lawyer present. Just presence. That’s the heart of medical consent. Not words. Not enthusiasm. Just truth. And sometimes, silence speaks louder than any "yes" ever could.
William Liu
December 30, 2025 AT 19:53People keep saying "yes means yes" like it’s a universal rule. But medicine isn’t a college party. It’s a hospital. And patients aren’t trying to avoid assault - they’re trying to survive. Let’s stop borrowing metaphors from one crisis to solve another. They’re not the same. And pretending they are? That’s not solidarity. That’s confusion with consequences.