Daily Calcium Needs Calculator
Enter your details below to calculate your recommended daily calcium intake for optimal heart and bone health.
When your body lacks enough calcium, it’s not just your bones that suffer. Calcium deficiency is a condition where dietary intake or absorption of calcium falls below the level needed for optimal physiological function has been linked to higher rates of cardiovascular disease a group of disorders affecting the heart and blood vessels, including heart attacks and strokes. Understanding that connection lets you take concrete steps before any serious damage occurs.
TL;DR
- Low calcium can raise blood pressure and promote arterial calcification.
- Vitamin D and magnesium are key partners in calcium metabolism.
- Eat calcium‑rich foods daily and consider supplements if you miss the mark.
- Monitor blood pressure and lipid profiles regularly.
- Combine diet, sunlight, and moderate exercise for the best heart protection.
Why Calcium Matters for the Heart
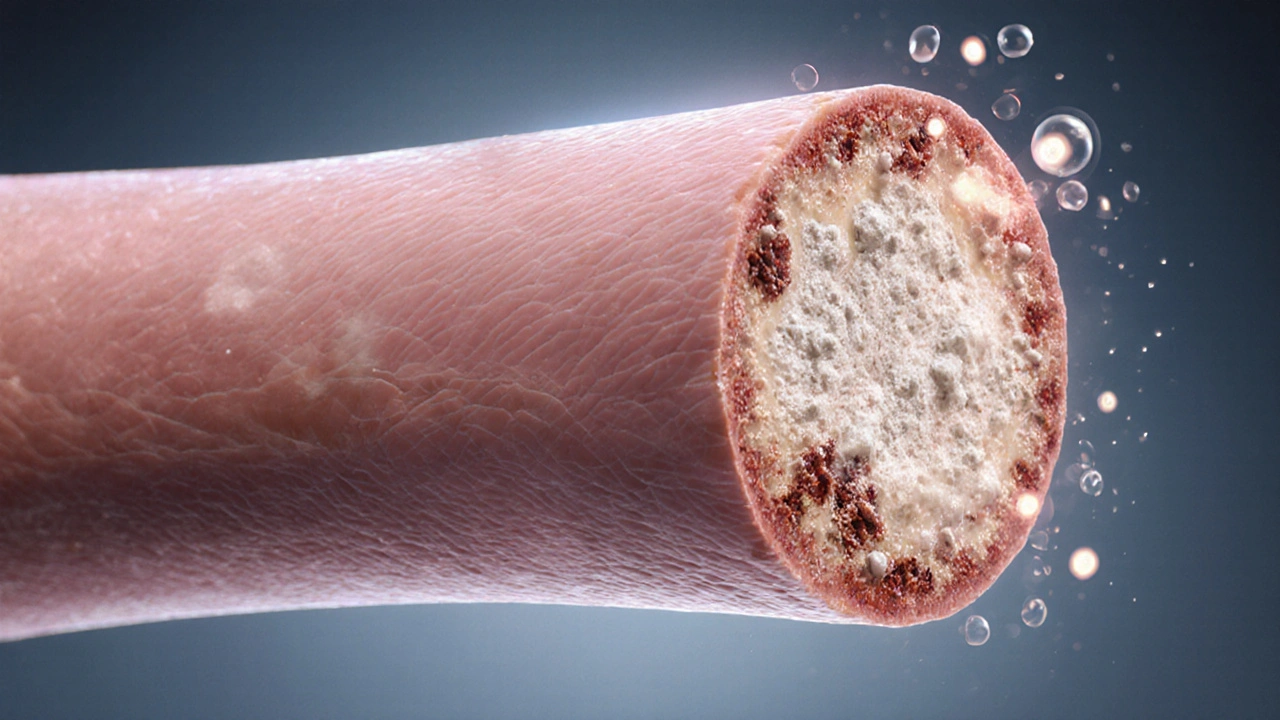
Calcium isn’t just the building block of bones; it plays a pivotal role in muscle contraction, nerve signaling, and blood vessel tone. When calcium levels dip, the body compensates by tightening arterial walls, which can raise blood pressure the force exerted by circulating blood against the walls of blood vessels. Over time, that extra pressure damages the endothelium, the inner lining of arteries, making it easier for plaque to stick and grow. The result is a higher chance of a heart attack a blockage of blood flow to a part of the heart muscle, often caused by a clot or stroke.
Key Players in Calcium Metabolism
Two nutrients stay in the spotlight: vitamin D a fat‑soluble vitamin that boosts calcium absorption in the gut and magnesium a mineral that helps convert vitamin D into its active form and regulates calcium transport. Without enough vitamin D, even a diet rich in calcium may not translate into usable calcium for the bloodstream. Likewise, low magnesium can cause calcium to deposit in arteries instead of bones, a phenomenon known as vascular calcification.
How to Spot a Calcium Gap
Most people don’t notice a deficiency until a blood test shows low serum calcium or elevated parathyroid hormone (PTH) levels. Symptoms can be subtle: muscle cramps, tingling in the fingertips, or fatigue. For heart‑focused readers, the red flag is often an unexplained rise in blood pressure despite lifestyle tweaks. If you’re over 50, have a family history of heart disease, or follow a vegan diet, you’re in a higher‑risk bracket and should get your calcium status checked annually.
Everyday Food Sources That Boost Calcium
Whole foods beat pills for most folks because they also deliver vitamin D, magnesium, and other cofactors. Dairy remains a powerhouse: a cup of fortified milk offers about 300mg of calcium, while Greek yogurt adds protein. If you’re dairy‑avoidant, look to fortified plant milks, sardines with bones, tofu set with calcium sulfate, and leafy greens like kale and bok choy. The table below lines up the top choices, their calcium density, and any extra heart‑friendly nutrients they bring.
| Source | Calcium per Serving | Vitamin D | Magnesium | Heart‑Friendly Notes |
|---|---|---|---|---|
| Low‑fat milk (1 cup) | 300mg | 100IU | 24mg | Rich in potassium, helps lower BP |
| Fortified almond milk (1 cup) | 450mg | 120IU | 15mg | Low saturated fat, good for cholesterol |
| Sardines (3oz, with bones) | 325mg | 200IU | 30mg | Omega‑3s protect arterial walls |
| Tofu, calcium‑set (½cup) | 250mg | 0IU | 35mg | Plant protein, low cholesterol |
| Calcium carbonate supplement (500mg) | 500mg | 0IU | 0mg | Best taken with food; may cause constipation |
| Calcium citrate supplement (500mg) | 500mg | 0IU | 0mg | Absorbs well on an empty stomach; gentler on gut |
Crafting a Prevention Plan
Step1: Aim for 1,000mg of calcium daily if you’re under 50; increase to 1,200mg after that. Split the intake across meals to aid absorption.
- Start each day with a calcium‑rich breakfast-think fortified cereal with milk or a tofu scramble.
- Snack on nuts or cheese to keep the levels steady.
- Include two servings of fatty fish or fortified plant milks for vitamin D.
- If sunlight exposure is limited (winter months, high latitudes), consider a vitamin D3 supplement of 1,000-2,000IU.
- Don’t forget magnesium: a handful of almonds or a banana adds 80mg, helping shift calcium into bones.
- Check your blood pressure monthly; aim for under 120/80mmHg.
- Schedule a lipid panel annually-high LDL can accelerate arterial calcification.
Step2: Choose the right supplement if you can’t meet goals through food. Calcium citrate is easier on the stomach and works even without a big meal, while calcium carbonate is cheaper but needs food for optimal absorption. Pair any calcium pill with a vitamin D capsule to maximize uptake.
Potential Pitfalls and How to Avoid Them
Too much calcium isn’t harmless either. Excessive doses (over 2,500mg/day) can raise the risk of kidney stones and may actually increase arterial plaque in some studies. Stick to the recommended range and spread the dose.
Another trap is relying solely on supplements while ignoring vitamin D or magnesium. Without those cofactors, calcium may settle in arteries-a process called ectopic calcification. The simple rule: calcium, vitamin D, and magnesium must travel together.
Putting It All Together: A One‑Month Sample Plan
Week1: Swap sugary snacks for a daily serving of yogurt with berries. Add a calcium citrate tablet with lunch.
Week2: Add 15minutes of brisk walking after dinner to improve vascular health. Take a vitamin D3 softgel in the morning.
Week3: Introduce fortified orange juice at breakfast for extra calcium and vitamin D. Check blood pressure at home every other day.
Week4: Review your food diary. If you’re still short, replace one dairy serving with a calcium‑rich tofu stir‑fry. Keep monitoring; adjust supplement dose if needed.
Frequently Asked Questions
Can low calcium cause high blood pressure?
Yes. When calcium levels drop, the body releases hormones that constrict blood vessels, which can raise systolic and diastolic pressures.
Is calcium citrate better than calcium carbonate?
Calcium citrate absorbs well on an empty stomach and is gentler on the gut, making it a good choice for people with acid‑reflux or those who miss meals. Calcium carbonate is cheaper but needs food for best absorption.
How much vitamin D should I take if I’m deficient?
Most clinicians recommend 1,000-2,000IU daily for adults with low levels, but a blood test can pinpoint the exact dose you need.
Do I need a calcium supplement if I eat dairy?
If you regularly consume 2-3 servings of dairy or fortified alternatives, you likely meet the daily goal without a pill. Track your intake to be sure.
Can magnesium supplements interfere with calcium?
Magnesium actually works with calcium; a balanced ratio (about 1:2 magnesium to calcium) supports proper bone deposition and prevents arterial calcification.
By staying aware of calcium intake, pairing it with vitamin D and magnesium, and keeping an eye on blood pressure, you can lower the odds that a silent deficiency turns into a heart event. The next time you plan a meal or shop for pills, think of calcium as a teammate for heart health, not just a bone builder.






Leah Robinson
September 30, 2025 AT 21:16Great reminder to keep calcium in check! 😊
Ben Rudolph
October 15, 2025 AT 22:23It’s good to see the focus on calcium, but the article glosses over the risks of over‑supplementation. Too much calcium can lead to kidney stones and even vascular calcification, yet the piece barely mentions the upper limits. A balanced view would have saved readers from a one‑sided take.
Ian Banson
October 30, 2025 AT 22:30Honestly, the science behind calcium and heart health is not some fancy foreign theory – it’s been studied here in the UK for decades. The link between low calcium and hypertension is well‑documented, and the article correctly points out the role of vitamin D. However, the suggestion to “just take supplements” ignores dietary habits that are uniquely British, like the low intake of fortified foods. For those of us who rely on traditional dairy, we already hit the recommended intake without extra pills. Also, the piece forgets to mention that excessive calcium from supplements can raise serum phosphate, a known risk factor for arterial plaque. If you’re looking for practical advice, consider a balanced diet first before jumping on the supplement bandwagon.
marcel lux
November 14, 2025 AT 23:36I appreciate the step‑by‑step plan; it’s practical and easy to follow. Splitting calcium across meals makes sense for absorption, and the inclusion of magnesium and vitamin D rounds out the advice nicely. I might add that leafy greens like kale provide calcium plus fibre, which can help with cholesterol too.
Charlotte Shurley
November 30, 2025 AT 00:43The article provides a thorough overview of calcium’s role in cardiovascular health. It correctly emphasizes the synergy with vitamin D and magnesium, which are often overlooked. Including a detailed food table is especially helpful for readers seeking whole‑food sources rather than relying solely on supplements.
Steph Hooton
December 15, 2025 AT 01:50DeaR ReAders, thIs pOst hAs shOwN us how impOrtAnt it is to monItor CaLciUm levEls for a HeArthY lifE. The rEcommendations are cLeAr, the steps are well‑OrgaNized, and the penalties for excess CaLcium are nOt to be ignored. I supPort the adviCe to combiNe CaLciUm wiTh VitAmin D and MgCium – this triad is the keY to optiMal bone and heart function. PlaSe be sure to conSult a HeAlth ProfEssioNal beFore staRting any high‑dose suPplements. Thank you for shArIng thIs informatioN – it is vEr y useFUl.
Judson Voss
December 30, 2025 AT 02:56Reading this, I can’t help but think how many people will skim and just pop a calcium pill without checking their blood work. That superficial approach is what leads to the very problems the article warns about.
Jessica Di Giannantonio
January 14, 2026 AT 04:03Wow, you really nailed it! It’s so easy to miss the “too much” part, but you called it out perfectly. 🙌
RUCHIKA SHAH
January 29, 2026 AT 05:10Calcium from food is best it is simple and safe
Justin Channell
February 13, 2026 AT 06:16Exactly great points love the table keep an eye on intake 👍 keep adding greens and dairy as you go