Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication errors. Many of these aren’t accidents-they’re the result of deeply held myths that sound harmless, even reasonable. You’ve probably heard them: "If one pill helps, two will help more." "Natural means safe." "I feel better, so I can stop taking it." These ideas are everywhere. But they’re not just wrong-they’re dangerous.
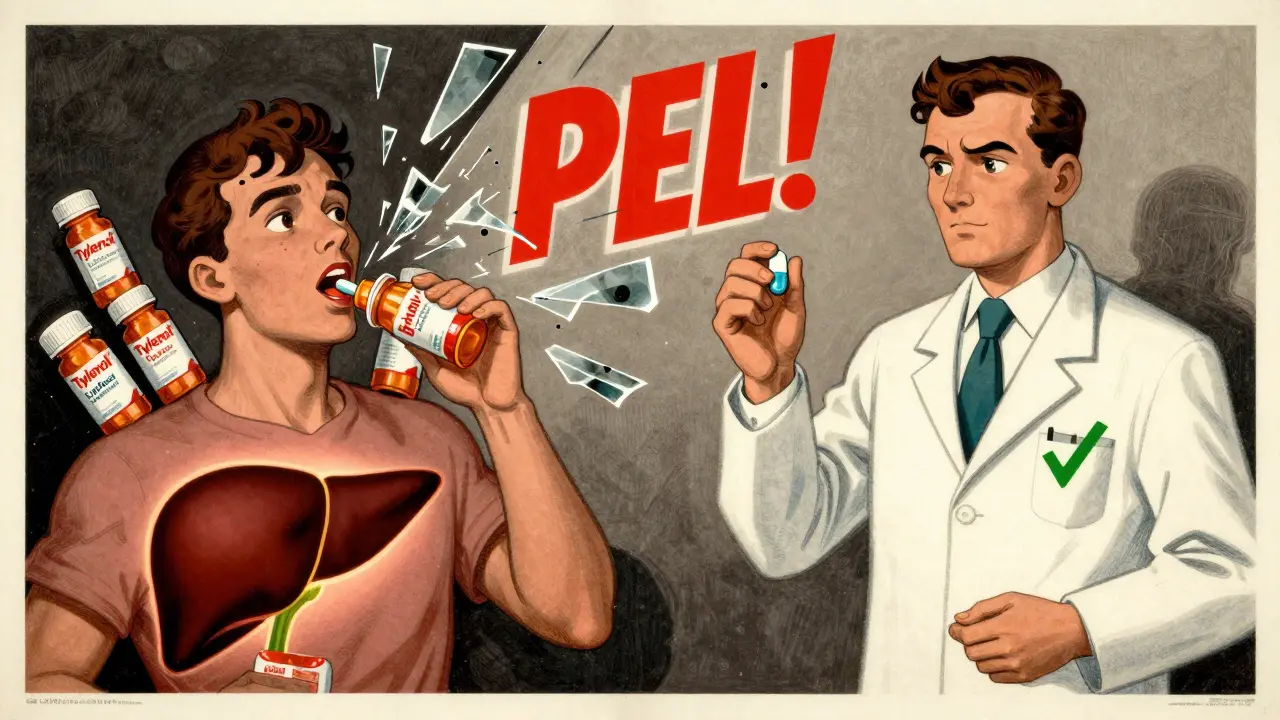
Myth: Over-the-Counter Medications Are Completely Safe
It’s easy to assume that if a drug doesn’t need a prescription, it can’t hurt you. But that’s one of the most deadly misunderstandings in medicine. Acetaminophen-the active ingredient in Tylenol and hundreds of other pain relievers and cold medicines-is the leading cause of acute liver failure in the U.S. The FDA lowered the daily limit to 3,000 mg in 2011 after years of data showed people were accidentally overdosing. How? By taking multiple products that all contain acetaminophen. A single extra-strength tablet has 500 mg. Eight of them hit 4,000 mg-past the safe limit. That’s enough to cause permanent liver damage or death. In 2022, acetaminophen overdose sent 56,000 people to the ER and killed 500. No prescription doesn’t mean no risk. Always check the active ingredients on every bottle you take.
Myth: Taking More Than the Recommended Dose Makes It Work Better
"I’m still in pain, so I’ll take another pill." This logic feels logical-until it isn’t. Ibuprofen, naproxen, and other NSAIDs don’t become more effective at higher doses. They just become more dangerous. A 2017 study in JAMA Internal Medicine found that taking more than 1,200 mg of ibuprofen in 24 hours increases the risk of gastrointestinal bleeding by 4.5 times. That’s not a small bump-it’s a massive jump. And it’s not just stomach issues. Higher doses can raise blood pressure, damage kidneys, and trigger heart problems. The dose on the label isn’t a suggestion. It’s the result of decades of research, clinical trials, and safety testing. More doesn’t mean better. It means risk.
Myth: You Can Stop Taking Medication Once You Feel Better
This myth is especially common with antibiotics. If your sinus infection starts clearing up after three days, why keep taking the pills? It seems smart. But stopping early is one of the biggest drivers of antibiotic resistance. The CDC estimates that 30% of antibiotic courses are stopped too soon. That’s not just your problem-it’s everyone’s. When you don’t kill all the bacteria, the toughest ones survive. They multiply. They spread. The result? Superbugs that no antibiotic can touch. In the U.S. alone, antibiotic-resistant infections cause 35,000 deaths each year. Completing your full course-even if you feel fine-isn’t about being obedient. It’s about survival.
Myth: Natural or Herbal Products Are Always Safe
"It’s natural, so it’s harmless." That’s a dangerous assumption. St. John’s Wort, a popular supplement for mild depression, can cut the effectiveness of birth control pills by up to 33%. That means unintended pregnancy. Ginkgo biloba, often taken for memory, increases bleeding risk by 50% when combined with warfarin-a blood thinner millions take. Even garlic supplements can thin your blood. The FDA doesn’t regulate supplements like prescription drugs. That means no standard dosing, no proven safety data, and no warning labels for dangerous interactions. Just because something comes from a plant doesn’t mean it’s safe with your other meds. Always tell your pharmacist or doctor what supplements you’re taking-even if you think they’re "just vitamins."

Myth: Mixing Alcohol with Prescription Medications Is Safe If You Don’t Drink Much
"I only have one glass of wine." That’s what many people say before they mix alcohol with opioids, sedatives, or even some antidepressants. But even small amounts can be deadly. A 2020 study in Addiction Biology found that combining alcohol with opioids like oxycodone or hydrocodone increases the risk of respiratory depression-when breathing slows to a stop-by 800%. That’s not a typo. It’s eight times more dangerous. Alcohol also boosts the sedative effects of sleep aids, anxiety meds, and muscle relaxants. The liver can’t process both at the same time. The result? Overdose, coma, or death. There’s no safe level of alcohol with many prescription drugs. If your medication label says "avoid alcohol," it’s not a suggestion. It’s a warning.
Myth: Generic Drugs Are Inferior to Brand-Name Ones
Some people believe generics are cheaper because they’re weaker. That’s false. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must be 80-125% bioequivalent-meaning they work the same way in your body. A 2022 analysis of 47 million prescriptions found no difference in effectiveness or safety between generics and brands for conditions like high blood pressure, diabetes, and depression. The only differences are in fillers, colors, or shape-none of which affect how the drug works. Choosing generics can save you hundreds a year without sacrificing safety or results.
What You Can Do: Five Proven Steps to Stay Safe
Knowing the myths isn’t enough. You need tools to protect yourself.
- Do a brown bag review. Every six months, bring all your medications-prescriptions, OTCs, vitamins, supplements-to your doctor or pharmacist. A 2021 study showed this cuts medication errors by 63%.
- Use the 5 Rights. Before taking any pill, ask: Is it the right patient (me)? The right drug? The right dose? The right route (swallowed, injected, etc.)? The right time? This simple check prevents most mistakes.
- Ask for the teach-back method. After your pharmacist explains your meds, say: "Can you please check if I understood correctly?" Then explain back what you’re supposed to take and why. A 2020 study found this boosts understanding from 42% to 89%.
- Sync your refills. If you take multiple meds, ask your pharmacy to align all your refills to one day each month. ExactCare Pharmacy’s program boosted adherence from 52% to 81% in just one year.
- Use trusted apps. Apps like Medisafe send reminders, track interactions, and alert you to dangerous combinations. Users saw a 37% drop in dosing errors.
Why This Matters: The Real Cost of Misinformation
Medication errors don’t just hurt individuals-they strain the whole system. Preventable adverse drug events cost the U.S. healthcare system $42 billion a year. One in five prescriptions dispensed in the U.S. involves a safety issue that a pharmacist could have caught-like a dangerous interaction or incorrect dose. The FDA’s new labeling rules for acetaminophen aim to prevent 5,000-10,000 liver injuries annually. AI-powered tools and pharmacist-led education are reducing errors, but only if patients listen. You’re not just a number on a chart. You’re the one who takes the pills. Your choices matter.
Final Thought: Your Meds Are Not a Guessing Game
Medication safety isn’t about being perfect. It’s about being informed. You don’t need to memorize every drug interaction. But you do need to ask questions. You need to challenge the myths you’ve heard since childhood. You need to speak up when something doesn’t feel right. The next time someone says, "It’s just a cold pill," or "I stopped my antibiotics because I felt fine," don’t nod along. Say: "Actually, that’s not safe." Because in medicine, the biggest dangers aren’t always the ones you see on the news. Sometimes, they’re the things we’ve always believed to be true.
Can I take two different over-the-counter pain relievers at the same time?
It depends. Many OTC pain relievers contain the same active ingredients. Taking two at once-like Tylenol and a cold medicine-can easily lead to an accidental acetaminophen overdose. Even if they seem different, always check the "Active Ingredients" section on the label. If both list acetaminophen, ibuprofen, or aspirin, don’t combine them. Use only one at a time, and stick to the maximum daily dose.
What should I do if I miss a dose of my medication?
Don’t double up unless your doctor or pharmacist says to. For most medications, if you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one. Doubling up can cause side effects or toxicity. Always check the medication guide or call your pharmacist-rules vary by drug.
Are herbal supplements safer than prescription drugs?
No. Herbal supplements aren’t held to the same safety and testing standards as prescription drugs. Many interact dangerously with medications. For example, St. John’s Wort can make birth control, antidepressants, and blood thinners ineffective. Ginkgo biloba increases bleeding risk. Just because something is "natural" doesn’t mean it’s safe. Always disclose supplements to your healthcare provider.
Why do some medications have black box warnings?
Black box warnings are the strongest safety alerts the FDA requires. They mean the drug carries a serious or life-threatening risk-like liver failure, heart attack, or suicidal thoughts. These warnings don’t mean you can’t take the drug-they mean you need to understand the risks and be monitored. Never ignore a black box warning. Ask your pharmacist to explain what it means for you.
Can I share my prescription medication with a family member who has similar symptoms?
Never. Even if symptoms seem the same, the cause might be different. A headache could be from stress, a sinus infection, or high blood pressure. Your medication is prescribed for your specific health profile, weight, allergies, and other drugs you take. Sharing prescriptions is illegal and can cause serious harm-or death. Always get your own diagnosis and prescription.
How do I know if my pharmacist is giving me the right advice?
A good pharmacist will ask you about all your medications, supplements, and health conditions. They’ll explain why you’re taking each drug, what side effects to watch for, and how to avoid interactions. If they just hand you the bottle without talking, ask for a consultation. Most pharmacies offer free medication reviews. You have the right to ask questions until you feel confident.
What’s the best way to store medications at home?
Keep them in a cool, dry place away from sunlight and moisture. The bathroom cabinet isn’t ideal-it’s humid. A locked drawer or cabinet in your bedroom is better. Always keep them out of reach of children and pets. Check expiration dates regularly. Discard expired or unused meds through a drug take-back program-don’t flush them unless the label says to.
Can I crush or split my pills if I have trouble swallowing them?
Only if your pharmacist says it’s safe. Some pills are designed to release medicine slowly. Crushing or splitting them can release the full dose at once, causing overdose. Others have coatings to protect your stomach or prevent bad taste. Always ask before altering your pills. There are often liquid versions or smaller tablets available.
Next Steps: What to Do Today
Don’t wait for a crisis. Take action now:
- Look at your medicine cabinet. Are there old pills you haven’t taken in months? Take them to a drug disposal site.
- Write down every medication, supplement, and OTC product you take. Bring it to your next appointment.
- Ask your pharmacist: "Are there any myths about my meds I should know?"
- Download a trusted medication app like Medisafe or MyTherapy and set up reminders.
Medication safety isn’t complicated. It’s about paying attention. It’s about asking questions. And it’s about refusing to believe the myths that could cost you your health.






Charlotte N
January 5, 2026 AT 13:20I never realized how many OTC meds have acetaminophen in them
My cold medicine had it and so did my pain pills
I just assumed they were different
Now I check every label like a hawk
Scary how easy it is to overdose without meaning to
Catherine HARDY
January 6, 2026 AT 09:15They're hiding the truth about pharmaceuticals
Big Pharma doesn't want you to know how dangerous their drugs really are
They profit off your ignorance
And now they're pushing generics like they're safe
But who really knows what's in them?
They could be cutting corners
Always trust your gut
Don't let them control your health
Chris Cantey
January 8, 2026 AT 03:19Medication safety is a myth designed to pacify the masses
The system doesn't care if you live or die
It cares about profit margins and liability shields
Doctors are trained to prescribe, not to question
Pharmacists are overworked and underpaid
And you? You're just a data point in a spreadsheet
Stop believing in systems
They're not your friends
Oluwapelumi Yakubu
January 8, 2026 AT 07:07Man, this post hit different in Nigeria
We don't even have access to half these meds
But when we do, people still think "natural" means safe
My cousin took moringa with his blood pressure pills and ended up in the hospital
Same story everywhere
Education is the real medicine here
And we need more of it
Not just in the US, but everywhere
Especially where pharmacies are just a guy with a plastic bag on the roadside
Knowledge saves lives, no matter the country
Jacob Milano
January 8, 2026 AT 19:23This is the kind of info that should be taught in high school
Not just in health class, but in every subject
Like, imagine if math class included calculating safe acetaminophen doses
Or biology covered herb-drug interactions
We'd have fewer ER visits
And fewer people dying from things they didn't understand
Thanks for laying this out so clearly
It's not scary because it's complex
It's scary because it's simple and we ignore it
And that's the real tragedy
saurabh singh
January 10, 2026 AT 08:32Bro, I used to think herbal stuff was always good
Then my uncle took ashwagandha with his heart meds and nearly had a stroke
Now I tell everyone: "If it's not in the pharmacy, ask before you take it!"
India has thousands of herbs, but we're not dumb about mixing them
We learned the hard way
Same rule applies here
Don't be cool with your health
Be smart
And if you're unsure?
Ask the pharmacist
They're the real superheroes
Not the influencers with gummies
Dee Humprey
January 11, 2026 AT 17:22I do the brown bag thing every 6 months now
My pharmacist remembers my name and my meds
She caught a dangerous combo I didn't even know about
It felt like she saved my life
And she didn't even charge me
Just smiled and said, "You're welcome, sweetie"
So if you're nervous about asking questions?
Just go
They want you to ask
They're not judging you
They're just waiting for you to show up
❤️
Jay Tejada
January 12, 2026 AT 19:30Yeah yeah, I know the myths are dumb
But let’s be real
Who actually reads the tiny print on the bottle?
Not me
Not most people
We’re busy
We’re tired
We just want the pain to go away
So yeah, the info’s good
But the real problem?
We’re not designed to be pharmacists
And nobody’s fixing that
Just saying
Allen Ye
January 13, 2026 AT 13:25There’s a deeper existential layer here
Medication safety isn’t just about chemistry or dosage
It’s about the collapse of trust in institutions
And the rise of individual responsibility in a world that never taught us how to bear it
We’re told to be autonomous agents
But given no tools to be informed ones
The myth of "natural" is a symptom of our spiritual hunger for purity in a synthetic world
And the dismissal of generics? That’s class anxiety disguised as health wisdom
We’re not just taking pills
We’re performing identity
And the cost? A body broken by ignorance
And a society too distracted to notice
Until it’s too late
mark etang
January 14, 2026 AT 16:37It is imperative that all individuals, regardless of socioeconomic status, educational background, or geographic location, be afforded equitable access to comprehensive pharmaceutical education. The dissemination of accurate, evidence-based information regarding medication safety is not merely a public health recommendation-it is a moral imperative. Failure to prioritize this constitutes a systemic dereliction of duty toward the citizenry. Immediate, scalable, and linguistically accessible interventions must be implemented across primary care, pharmacy, and digital platforms to mitigate preventable harm. The time for passive compliance has expired. Proactive, structured, and universally enforced patient education is not optional. It is non-negotiable.