When a drug’s patent runs out, prices don’t just dip-they often collapse. It’s not magic. It’s economics. For years, a single company sells a medicine at a high price because they’re the only one allowed to make it. Then, the patent expires. Suddenly, dozens of other companies jump in. And the price? It can fall by 80% or more within a few years. This isn’t theoretical. It’s happening right now with drugs like Eliquis, Humira, and Ozempic.
What Happens When a Patent Expires?
A pharmaceutical patent gives a company exclusive rights to sell a drug for about 20 years from the date it was filed. But that’s not the full story. Most drugs spend 5-10 years in clinical trials before they even hit the market. So the real window of monopoly pricing is often just 10-12 years. Once that ends, any company can apply to the FDA (or equivalent agencies) to make a generic version. The first generic maker usually brings the price down by 15-20%. That’s noticeable. But the real drop comes when the second, third, and tenth generics arrive. By the time 10 or more companies are selling the same drug, prices can plunge to 80-90% below the original. In the U.S., the average price for a drug falls 32% in the first year after patent expiry and 82% over eight years, according to a 2023 JAMA Health Forum study of 505 drugs across eight countries.Why Do Prices Drop So Much?
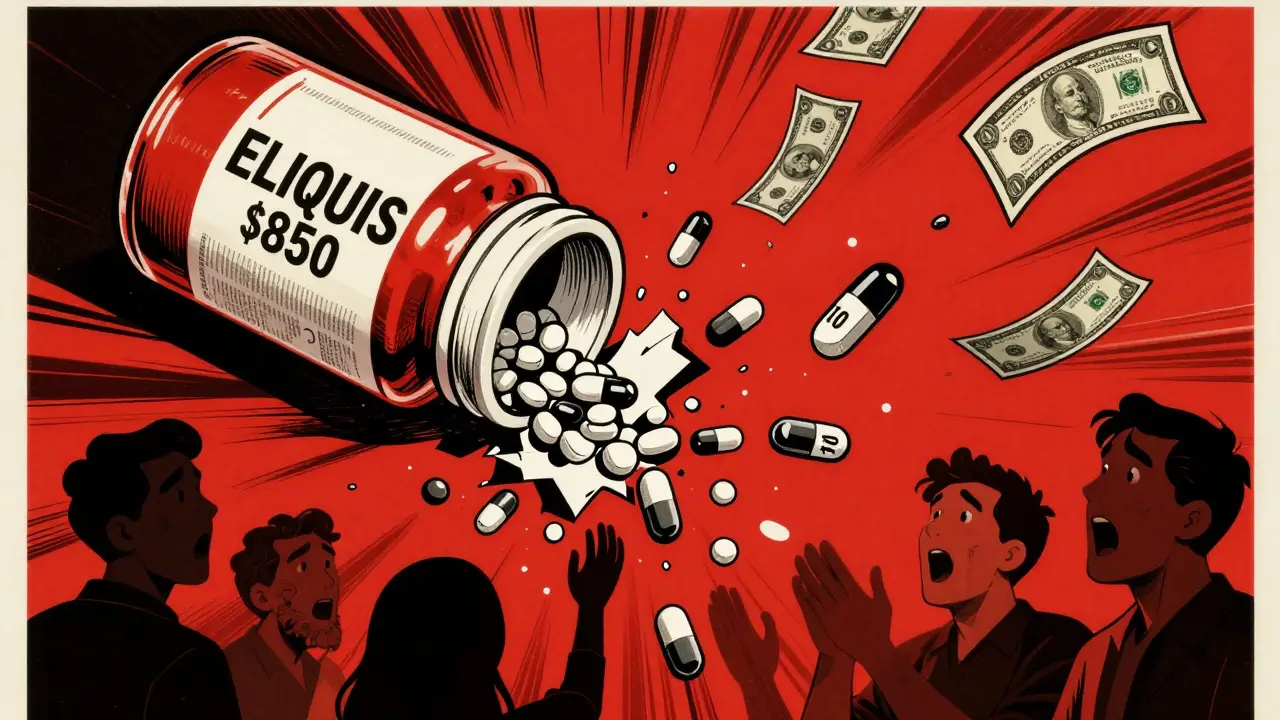
It’s simple competition. When only one company sells a drug, they set the price. No one else can compete. But once generics enter, it becomes a race to the bottom. Generic manufacturers don’t need to spend millions on clinical trials-they just have to prove their version works the same way. That cuts their costs dramatically. The more competitors, the harder they fight to win pharmacy contracts. Hospitals and insurers want the cheapest option. So generics undercut each other. In the U.S., a drug that cost $850 a month as a brand-name product can drop to $10 a month as a generic. That’s what happened with Eliquis (apixaban) after its patent expired in 2020. Patients on Reddit reported paying $850 before and $10 after. That’s not a typo.Not All Drugs Are Created Equal
Small-molecule drugs-like aspirin, statins, or blood thinners-are easy to copy. Their chemical structure is simple. So generics enter fast, and prices crash quickly. Biologics are different. These are complex drugs made from living cells-like Humira (adalimumab) or Ozempic (semaglutide). Copying them isn’t as simple as making a pill. The generic versions are called biosimilars, and they take longer to approve, cost more to develop ($2-5 million per product), and face more legal hurdles. That’s why Humira’s price didn’t drop until 2023-seven years after its main patent expired. AbbVie, the maker, filed over 130 secondary patents on minor changes, delaying competitors. Even when biosimilars finally arrive, prices don’t always fall right away. Some drugmakers use rebate deals with insurers to keep the brand-name drug on the preferred list. So patients might still pay full price, even if a cheaper biosimilar exists. A 2023 Kaiser Family Foundation survey found 22% of insured adults saw delays in accessing lower-cost alternatives because of these formulary tricks.
Global Differences: Why Prices Fall Faster in Some Countries
The U.S. isn’t the only country dealing with patent expirations-but it’s the one where prices drop the most. Why? In the U.S., drug prices are set by the market. Insurers and pharmacies negotiate directly with manufacturers. When generics come in, they win by being cheaper. No government price controls. So competition drives prices down hard. In Europe, governments set prices. They use reference pricing-meaning if a drug is cheaper in Germany, France will match it. That slows the drop. In Switzerland, prices barely budged after patent expiry-only 18% lower after eight years. Australia saw a 64% drop. The UK and Canada were around 60%. The timing of generic entry also varies. In the U.S., generics typically arrive 30 months after patent expiry. In Europe, it’s often 12-18 months. That delay costs patients billions.The Hidden Game: Patent Thickets and Evergreening
Drug companies don’t wait for patents to expire before planning their next move. They file secondary patents on tiny changes-new dosages, delivery methods, or packaging. This is called “evergreening.” The R Street Institute found that 78% of new patents filed for drugs between 2010-2020 weren’t for new medicines. They were for old ones with minor tweaks. For example, semaglutide (Ozempic, Wegovy) has 142 patents covering different formulations. Even though the base patent expires in 2026, these secondary patents could extend exclusivity until 2036. I-MAK’s 2025 report says the average blockbuster drug gets 10-15 secondary patents, extending market control by 12-14 years. That’s not innovation. It’s legal strategy. The FDA approved 870 generic drugs in 2023-up 12% from 2022. But many of those are still stuck waiting because of patent litigation or complex approval processes for biosimilars.






Ellie Stretshberry
December 26, 2025 AT 15:03i just paid $12 for my apixaban script last week
last year it was $800
my heart is so much lighter now
Zina Constantin
December 27, 2025 AT 04:45THIS IS WHY WE NEED TO SUPPORT GENERIC DRUGS. The system isn't broken-it's just been hijacked by corporate loopholes. Every time a patent expires and prices drop, it's a win for real people, not shareholders. We should celebrate this like a holiday. Imagine if we applied this logic to insulin, or asthma inhalers, or even mental health meds. The power of competition is real, and it's beautiful.
Dan Alatepe
December 29, 2025 AT 04:01yo i live in nigeria and we don't even get these drugs at all 😭
if we do, it's $500 a bottle and no generics
so i'm happy for you guys but also... why is this a privilege? 🤡
Angela Spagnolo
December 29, 2025 AT 21:57...I just read this again... and I'm crying. Not because I'm sad... but because I finally feel seen. I've been on Humira for 7 years. The price used to be $12,000 a year. Now? $1,200. And I didn't even know it was possible. Thank you for writing this. It's not just numbers-it's life.
Sarah Holmes
December 30, 2025 AT 13:59Let me be perfectly clear: this is not 'economics.' This is systemic exploitation disguised as innovation. These corporations spent decades convincing the public that drugs are 'miracles' while they engineered patent cliffs to maximize profit. The FDA is complicit. The AMA is complicit. And now, when the inevitable happens-prices drop-they pretend it's a 'market victory.' It's not. It's justice. Overdue, but justice nonetheless.
Jay Ara
December 31, 2025 AT 21:45in india we get generics fast and cheap
my dad takes metformin for 5 rupees a pill
you guys in usa pay 100x for same thing
its not about science its about greed
Kuldipsinh Rathod
January 2, 2026 AT 09:08my cousin in pharma told me biosimilars take 5-7 years to get approved here
in europe they do it in 18 months
why? because we let lawyers write the rules not doctors
SHAKTI BHARDWAJ
January 3, 2026 AT 13:42you all are so naive
the drug companies just made a new version of ozempic with a different name and raised the price again
they dont care about patents they care about your wallet
you think this is progress? its just the same scam with new packaging
Matthew Ingersoll
January 3, 2026 AT 19:23Patent expiration is one of the few natural checks on corporate power in pharmaceuticals. The fact that it’s so fiercely resisted speaks volumes. The real question isn’t why prices drop-it’s why they were ever this high to begin with.
Jody Kennedy
January 4, 2026 AT 05:02OMG I just realized-my insurance didn’t even tell me I could switch to the generic for Eliquis! I’ve been paying $800 for nothing for a year. I’m calling them right now. Thank you for this post. You just saved me a fortune 💪
wendy parrales fong
January 6, 2026 AT 04:47it’s funny how we treat medicine like a luxury item
we don’t do this with water or electricity
but somehow a pill that keeps you alive is treated like a designer handbag
maybe we need to stop thinking of health as a product and start thinking of it as a right
just saying
Lori Anne Franklin
January 6, 2026 AT 22:15i just got my 30-day supply of atorvastatin for $3
used to be $120
and i’m just sitting here thinking... how many people died because they couldn’t afford it before?
and how many more still can’t?
we need to fix this system
Bryan Woods
January 7, 2026 AT 08:56Thank you for the comprehensive breakdown. The data presented in the JAMA Health Forum study and the Congressional Budget Office projections are critical for public policy discourse. The systemic delay in generic entry due to patent thickets represents a significant market distortion that warrants legislative intervention. This is not merely a pharmaceutical issue-it is a socioeconomic imperative.