Switching from brand-name immunosuppressants to generics can save thousands of dollars a year - but for transplant patients, that savings might come with a dangerous risk. Cyclosporine and tacrolimus aren’t just any medications. They’re life-saving drugs with a razor-thin margin between working and failing. One milligram too little, and your body may reject the new organ. One milligram too much, and your kidneys or liver could start shutting down. This isn’t theoretical. Real people have been hospitalized after switching to a different generic version of these drugs.
Why These Drugs Are So Different From Other Generics
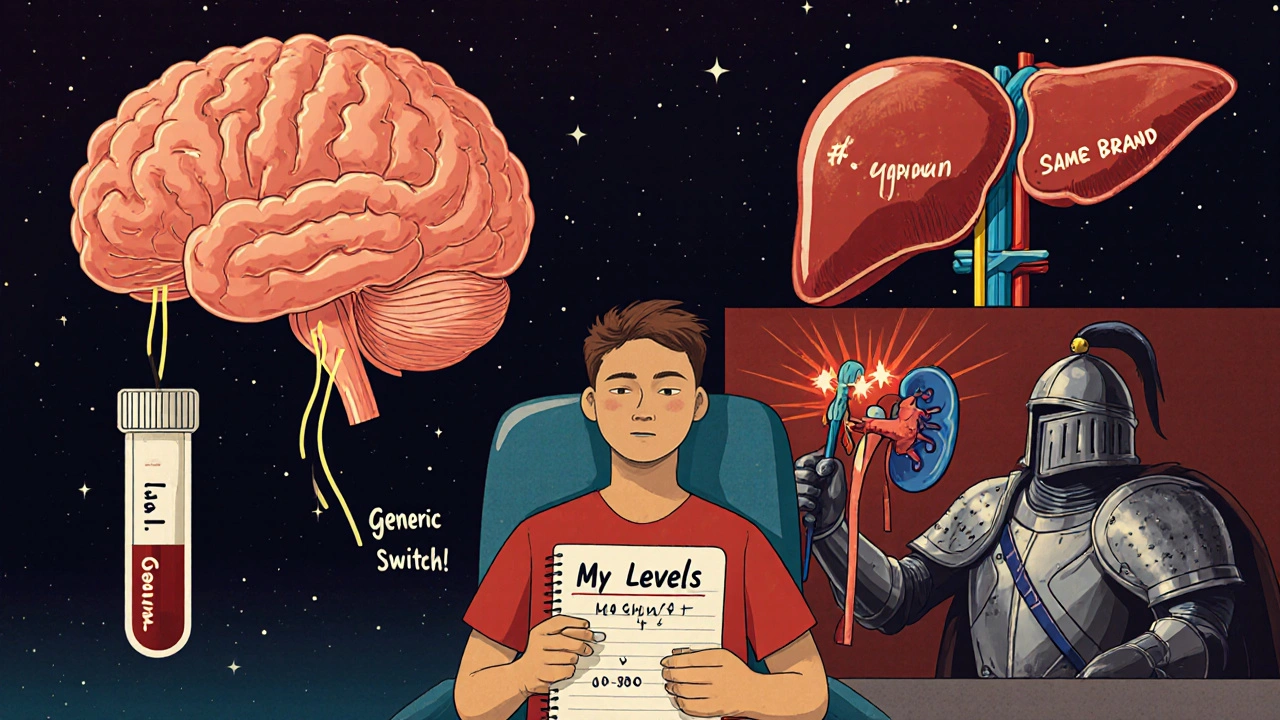
Most generics are straightforward swaps. A generic ibuprofen works just like Advil. But cyclosporine and tacrolimus are narrow therapeutic index (NTI) drugs. That means the difference between a safe, effective dose and a toxic or ineffective one is tiny. For tacrolimus, the target blood level is between 5 and 15 ng/mL. Go below 5, and rejection risk spikes. Go above 15, and you risk kidney damage, tremors, or even seizures. The problem isn’t that generics are fake. They’re approved by the FDA. But bioequivalence standards for NTI drugs are too loose. The FDA allows generics to vary by up to 25% in how much of the drug enters your bloodstream compared to the brand. For most pills, that’s fine. For tacrolimus, a 25% drop in absorption could mean your blood level falls from 10 ng/mL to 7.5 - still within the "normal" range, but close enough to the edge that rejection becomes possible.Cyclosporine vs. Tacrolimus: The Clinical Reality
Tacrolimus replaced cyclosporine as the go-to drug for most transplant centers after studies showed it cut rejection rates nearly in half. In one major trial, only 19.6% of patients on tacrolimus had acute rejection in the first six months - compared to 37.3% on cyclosporine. Graft survival was better, kidney function improved, and fewer patients needed extra anti-rejection drugs. But tacrolimus isn’t perfect. It’s linked to a higher chance of developing diabetes after transplant - nearly 20% of patients, versus 4% on cyclosporine. It also causes more tremors, headaches, and tingling in the hands and feet. Cyclosporine, while less effective at preventing rejection, tends to cause more hair growth, gum swelling, and high blood pressure. The real issue? Both drugs are now mostly generic. In the U.S., over 92% of prescriptions for these drugs are generic. That’s great for cost - generic tacrolimus costs $300-$500 a month, while the brand Prograf used to cost over $1,200. Generic cyclosporine runs $150-$300, down from $800-$1,000 for Neoral. But the savings come with a hidden price: inconsistency.Why Generic Switches Cause Problems
Not all generic versions are made the same. One manufacturer’s tacrolimus capsule might use a different oil base, filler, or coating than another’s. These small differences change how the drug dissolves in your gut. That changes how much gets absorbed. And since your body absorbs tacrolimus in a highly variable way to begin with - influenced by food, gut health, and other meds - adding a new generic into the mix is like throwing a wrench into a finely tuned machine. Transplant patients have reported dramatic drops in blood levels after switching generics. One patient on Reddit saw their tacrolimus level plunge from 8.5 ng/mL to 5.2 ng/mL within two weeks after switching from one generic to another. That’s not a fluke. It led to a biopsy-proven rejection episode. Another patient had to be hospitalized after their cyclosporine levels became unpredictable with a new generic brand. A 2022 survey of transplant patients found that 42.7% noticed new or worsening side effects after switching to generic immunosuppressants. Nearly 1 in 5 needed a dose adjustment because their blood levels became unstable.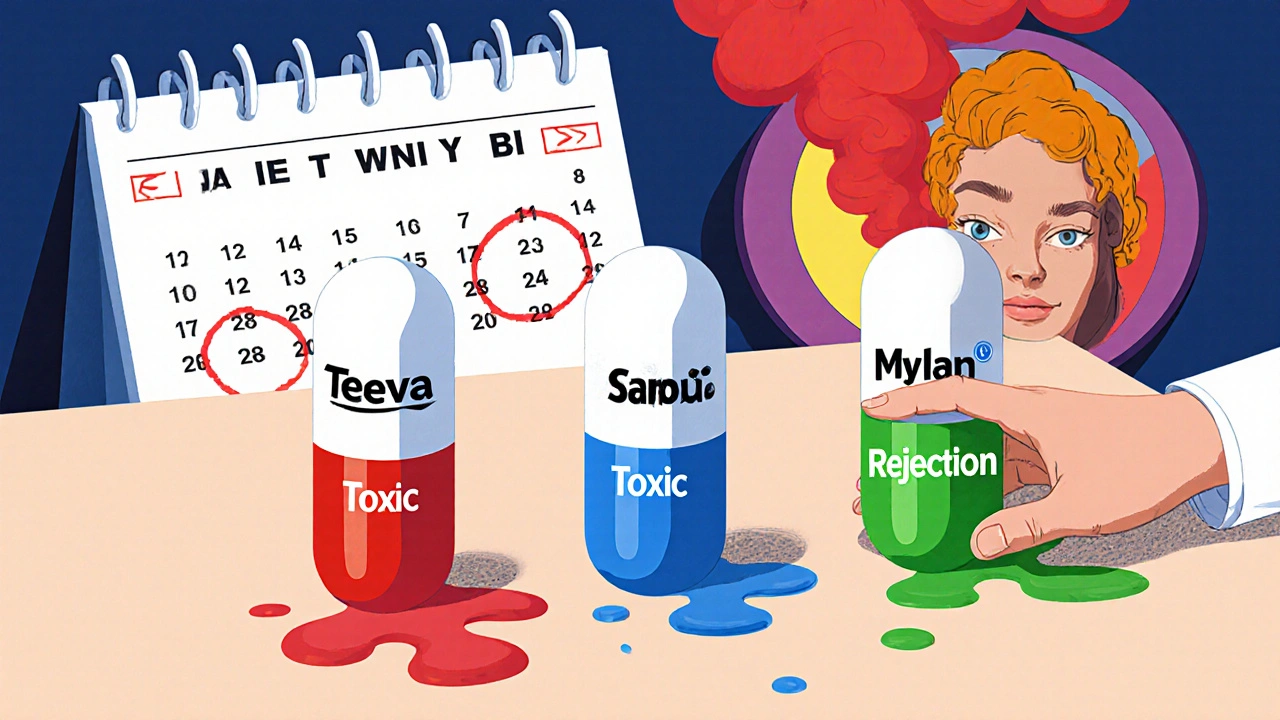
What Doctors and Pharmacies Are Doing About It
Most transplant centers now have strict rules about generic switches. Many won’t let patients switch between different generic brands unless absolutely necessary. Some hospitals sign contracts with a single generic supplier - meaning every patient gets the same version, year after year. This reduces variability and makes monitoring easier. Pharmacists are trained to flag any switch. If you’re on a generic tacrolimus made by Teva and your insurance forces a switch to Mylan, your transplant team will likely require weekly blood tests for four to six weeks. They’ll watch your levels like a hawk. If your numbers dip or spike, they’ll adjust your dose - or switch you back. The American College of Clinical Pharmacy recommends this protocol: Never switch generics without monitoring. Never switch back and forth. Always stick to one generic version if it’s working.What You Can Do to Stay Safe
If you’re on cyclosporine or tacrolimus, here’s what you need to know:- Know your generic brand. Check the pill’s imprint code or ask your pharmacist. Write it down. If your prescription changes, ask if it’s the same manufacturer.
- Never switch without telling your transplant team. Even if your insurance forces a switch, contact your doctor or pharmacist first. Don’t assume it’s safe.
- Get your blood levels checked after any switch. Don’t wait for symptoms. Test within 1-2 weeks after a new generic starts.
- Avoid grapefruit and Seville oranges. These interfere with how your body breaks down both drugs, making levels unpredictable.
- Take your dose at the same time every day. Even a 2-hour shift can affect absorption.
- Keep a log. Track your doses, blood levels, and any new symptoms. Bring it to every appointment.
The Bigger Picture: Cost vs. Safety
The push for generics is understandable. Transplant care is expensive. Medicare Part D and private insurers want to cut costs. And yes - many patients switch to generics without any issues. One user on HealthUnlocked said they’ve been on a generic tacrolimus for 18 months with perfect levels and no problems. They saved $900 a month. But for others, the cost savings aren’t worth the risk. The U.S. Renal Data System found that patients on generics were 15.3% more likely to miss doses - not because they were careless, but because they feared the drugs weren’t working the same way. The European Medicines Agency and the International Transplant Society both warn against routine switching between generic brands. They say the risk of rejection or toxicity isn’t worth the savings if you can avoid it.What’s Changing Now
Newer formulations are trying to fix the problem. In late 2023, the FDA approved a new extended-release version of tacrolimus (LCP-tacrolimus) that releases the drug slowly, reducing peaks and valleys in blood levels. This could make generic switches safer in the future. Some researchers are also using genetic testing. About half of people have a gene variant (CYP3A5) that makes them metabolize tacrolimus faster. If you’re one of them, you might need a higher dose - regardless of which generic you’re on. Testing for this before starting the drug can help personalize dosing and reduce the risk of instability.Bottom Line: Don’t Take It Lightly
Cyclosporine and tacrolimus aren’t like antibiotics or blood pressure pills. You can’t just swap generics and hope for the best. These drugs demand precision. Your body’s immune system is watching every tiny change in drug level. A small drop might mean your new kidney is under attack. A small spike might mean your liver is being poisoned. Generic versions are a tool - not a free pass. They can save money. But they must be used carefully. The safest path? Stick with one generic brand. Test your levels after any change. Communicate with your care team. And never assume that "generic" means "identical."Can I switch between different generic versions of tacrolimus safely?
No, not without close monitoring. Switching between different generic brands of tacrolimus can cause your blood levels to drop or spike, increasing the risk of organ rejection or toxicity. Most transplant centers require weekly blood tests for 4-6 weeks after any switch. Always talk to your transplant team before switching.
Why is tacrolimus more dangerous than cyclosporine when switching generics?
Tacrolimus has a narrower therapeutic window - its effective range is 5-15 ng/mL, compared to cyclosporine’s 100-200 ng/mL. A 10% change in absorption for tacrolimus can push you out of the safe zone. Cyclosporine’s wider range gives more room for error. Also, tacrolimus is absorbed less predictably in the gut, making it more sensitive to formulation changes.
How do I know which generic version I’m getting?
Check the pill’s imprint code (letters or numbers printed on it) or ask your pharmacist for the manufacturer’s name. Common generic makers include Teva, Mylan, Sandoz, and Apotex. Write down the name and look it up if you’re unsure. If your prescription changes without warning, call your pharmacy and transplant team immediately.
Should I avoid generics altogether and stick with brand-name drugs?
Not necessarily. Many patients do fine on generics - especially if they stay on the same brand. The issue isn’t generics themselves, but switching between them. If your current generic works and your levels are stable, keep it. If you’re forced to switch, insist on monitoring. Brand-name drugs are expensive, and most insurance won’t cover them unless you’ve tried generics first.
What should I do if I feel different after switching to a new generic?
Don’t wait. Contact your transplant team right away. Symptoms like unexplained fatigue, tremors, headaches, swelling, or changes in urine output could signal a drug level problem. Request a blood test immediately. Keep a symptom log and bring it with you. Your life depends on catching changes early.
Are there any foods or supplements I should avoid with these drugs?
Yes. Grapefruit, Seville oranges, pomelos, and starfruit can block the enzyme (CYP3A4) that breaks down both drugs, causing levels to rise dangerously. Avoid them completely. Also avoid St. John’s wort, which can lower levels and trigger rejection. Always check with your pharmacist before starting any new supplement or herb.


Mark Kahn
November 20, 2025 AT 12:10Just wanted to say thanks for laying this out so clearly. I’m on generic tacrolimus and had no idea how delicate the balance was. My doc never explained the absorption stuff - just said "take it like usual." Now I’m checking my pill imprint every time I refill. Seriously, this saved me from a potential disaster.
Leo Tamisch
November 21, 2025 AT 19:51How quaint. We’ve reduced life-saving medicine to a commodity, then acted surprised when the system crumbles under its own weight. The FDA’s 25% bioequivalence allowance for NTI drugs isn’t just lazy - it’s a moral failure disguised as fiscal prudence. 🤦♂️
Daisy L
November 23, 2025 AT 02:16THIS. IS. NON-NEGOTIABLE. I don't care if your insurance wants to save $900/month - your kidney doesn't care about your deductible! Switching generics is like swapping out the engine in your brain's security system and hoping it still works. NOPE. NOPE. NOPE!!!
Eliza Oakes
November 24, 2025 AT 14:30Oh please. Everyone’s acting like this is new. I’ve been on cyclosporine since 2015. Switched generics five times. Never had an issue. People just panic because they don’t understand pharmacokinetics. Maybe stop Googling and start listening to your nephrologist?
Shawn Sakura
November 25, 2025 AT 00:19Hey, I’m not a doctor, but I’ve been on tacrolimus for 7 years now. Started on brand, switched to Teva, stayed there. My levels are rock solid. Just don’t switch brands randomly, and always get tested after any change. You got this. 💪 And yeah - grapefruit is the devil. 🍊❌
Swati Jain
November 26, 2025 AT 15:04Let’s be real - this isn’t about generics. It’s about systemic neglect in transplant care. Pharma companies design formulations to exploit regulatory loopholes, insurers force switches like it’s a game of musical chairs, and patients are left holding the bag. 🇮🇳 We don’t do this in our hospitals back home - why here?
Florian Moser
November 28, 2025 AT 03:27Consistency is everything. If your current generic works - stick with it. If you must switch, insist on weekly blood tests for six weeks. Document everything. Communicate proactively. This isn’t just medical advice - it’s survival protocol. Your transplant team is your lifeline. Use them.
jim cerqua
November 28, 2025 AT 10:37My sister’s kidney failed six months after switching from Teva to Mylan. Her levels dropped from 9.1 to 4.8. Biopsy showed acute rejection. She had to go back on dialysis for 8 months before getting a second transplant. This isn’t a "risk." It’s a tragedy waiting to happen - and it’s happening EVERY. SINGLE. DAY. 🚨
Cooper Long
November 30, 2025 AT 10:28The issue is not generic drugs. It is the lack of standardized labeling and mandatory monitoring protocols. The FDA approves bioequivalence - but does not mandate post-market surveillance for NTI drugs. This gap must be addressed at the regulatory level.
Logan Romine
December 2, 2025 AT 03:30So… we’re saying a pill made in India with different fillers is suddenly a death sentence? 😂 I mean, if you’re this scared of your meds, maybe you shouldn’t have gotten the transplant in the first place. Just saying.
Franck Emma
December 3, 2025 AT 15:13I lost my liver because they switched me without telling me. No warning. No test. Just a new bottle. Now I’m on the waiting list again. And the worst part? They still make me take the generic.
Noah Fitzsimmons
December 5, 2025 AT 12:45You’re all overreacting. I switched generics three times last year. My levels? Perfect. My doctor? Laughed. You people treat these drugs like they’re magic spells. They’re not. They’re chemistry. Learn it. Stop crying.