When your hospital runs out of morphine, or the IV antibiotics for a patient with sepsis don’t arrive, you don’t have time to panic. You have to act. Medication shortages aren’t rare anomalies anymore-they’re a daily reality in hospitals across the U.S. and beyond. In 2022, the FDA tracked 287 drug shortages, affecting nearly one in five essential medications used in hospitals. And it’s not just about running out of stock. It’s about patients waiting longer for treatment, nurses working extra shifts, and doctors making life-or-death choices because the right drug simply isn’t there.
Why Do Medication Shortages Keep Happening?
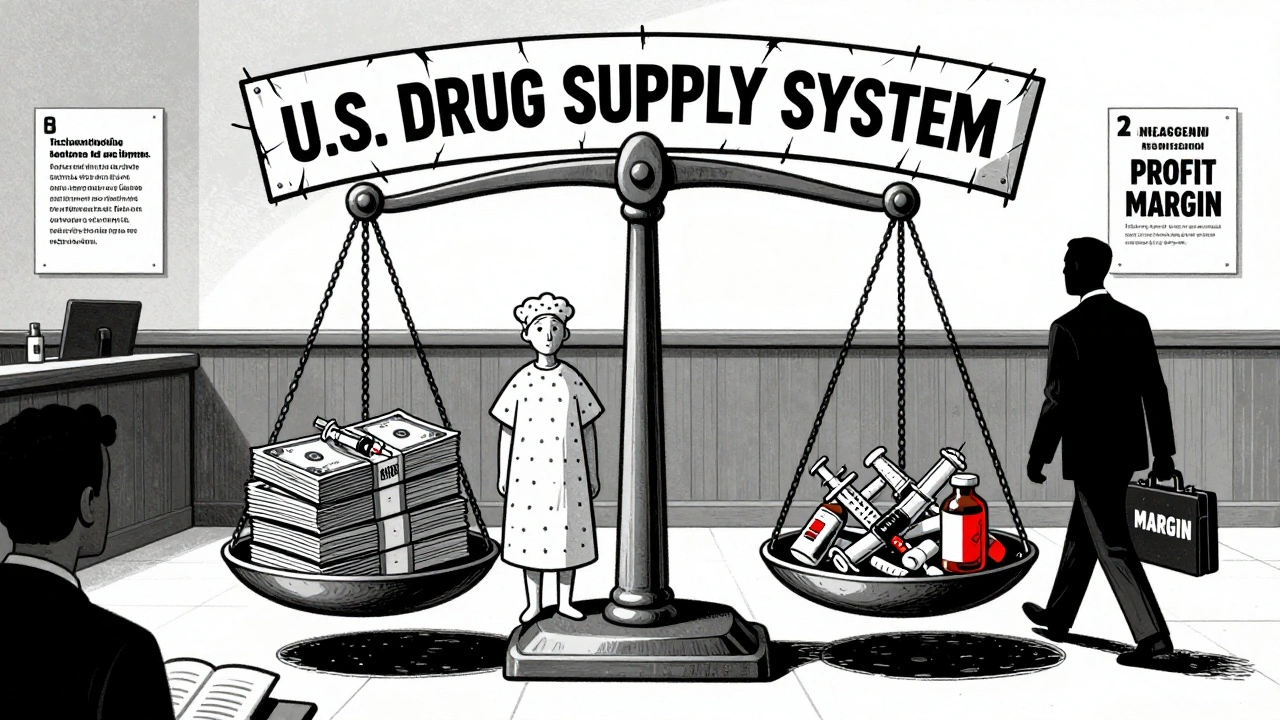
The root causes aren’t complicated, but they’re deeply systemic. Over 60% of all drug shortages involve generic sterile injectables-things like saline, morphine, antibiotics, and cancer drugs. These aren’t flashy, high-margin medications. They’re cheap, simple to make, and produced by just a handful of manufacturers. In fact, three companies control 75% of the global supply for these critical drugs. If one plant has a quality issue, the whole system stumbles.
Quality problems are the biggest culprit. In 2022, 46% of shortages were caused by manufacturing failures-contaminated batches, equipment breakdowns, or failure to meet FDA standards. These aren’t random glitches. They’re often the result of underinvestment. Many generic drug makers operate on razor-thin margins, especially when Medicaid and 340B rebate programs cap what they can charge. There’s little financial incentive to upgrade equipment, hire more staff, or build backup systems.
And then there’s the global supply chain. About 80% of the active ingredients in U.S. drugs come from overseas-mostly China and India. A single factory shutdown due to weather, labor issues, or regulatory action can ripple across the country. A shortage that starts in a plant in Hyderabad can mean a cancer patient in Chicago waits weeks for their next dose.
Who Gets Hit the Hardest?
It’s not evenly distributed. Rural hospitals, safety-net clinics, and facilities serving Medicaid or uninsured patients feel the pinch the most. A 2023 study from the American College of Physicians found that 78% of these facilities had to cancel or delay procedures because they couldn’t get the drugs they needed. Meanwhile, large urban hospitals with bigger budgets and more negotiating power often find alternatives first.
Patients on long-term chemotherapy, those in intensive care, and people with chronic pain are especially vulnerable. When morphine runs out, nurses scramble to substitute hydromorphone. But that’s not a simple swap. Dosing is different. Side effects vary. In one hospital, medication errors jumped 15% during a morphine shortage. Patients didn’t get the right amount. Some got too much. Others didn’t get enough.
And it’s not just about the drug itself. It’s about the workflow. Nurses report waiting an extra 22 minutes on average just to get a critical medication delivered. That’s 22 minutes a patient spends in pain, in distress, or at risk of deterioration. Pharmacists are working 12.7 extra hours a week just to manage shortages. One pharmacy director told a researcher, “We learn about shortages when the truck doesn’t show up. By then, it’s too late.”
What Can Hospitals and Pharmacies Do Right Now?
Waiting for Congress to fix the system isn’t an option. The tools to manage shortages are already here-they just need to be used.
- Build a shortage response team. It’s not just pharmacists. You need nurses, IT staff, risk managers, finance officers, and communications leads. They should meet weekly during normal times-and be called within four hours when a shortage hits. One hospital in Minnesota cut medication errors by 33% after starting weekly simulations.
- Track everything. Keep a real-time log: when the shortage was identified, what alternatives were considered, who approved them, how many errors occurred, and how long the shortage lasted. Data isn’t just for reports-it’s for learning.
- Stock smart, not just more. The American Society of Health-System Pharmacists recommends keeping 14 to 30 days of buffer stock for critical drugs. But most safety-net hospitals can only afford 8 to 12 days. Even a few extra days can buy time to find alternatives or reorder.
- Train for the unexpected. Quarterly drills should include mock shortages. Practice switching from one drug to another. Simulate what happens if the backup isn’t available. Teams that train for this perform better under pressure.
Some hospitals have started using software that flags potential shortages before they’re officially announced. If a manufacturer reports a production delay to the FDA, that information can show up in hospital systems within hours-not days. Proactive monitoring cuts response time in half.

What Are the Best Alternatives?
Not every drug has a direct substitute. But many do. The trick is knowing which ones are safe, effective, and available.
For example:
- If vancomycin is unavailable, linezolid or daptomycin may work for certain infections-but only if the patient’s kidney function and infection type allow it.
- When epinephrine auto-injectors run out, some clinics have switched to pre-filled syringes with strict protocols for administration.
- For propofol shortages in anesthesia, ketamine or midazolam can be used in combination, but require more monitoring.
Always check clinical guidelines. The American Society of Health-System Pharmacists and the Institute for Safe Medication Practices publish updated alternative lists regularly. Don’t guess. Don’t rely on memory. Use validated resources.
And remember: substitution isn’t just about matching the drug class. It’s about matching the patient. A 70-year-old with heart failure might not tolerate the same alternative as a 30-year-old athlete. Always assess risk versus benefit.
Why the U.S. System Is Falling Behind
Other countries handle this better. In Germany, they maintain national stockpiles of critical drugs. When a shortage hits, they release supplies from reserve. In France and Canada, manufacturers are legally required to report potential shortages months in advance. That gives hospitals time to plan.
In the U.S., reporting is voluntary. Only 65% of manufacturers comply. And even when they do, the FDA doesn’t have the power to force production or allocate supplies. There’s no national stockpile for everyday drugs-just the Strategic National Stockpile, which is meant for bioterrorism or pandemics, not routine insulin or saline shortages.
The economic model is broken. Generic drug makers can’t raise prices to cover costs because Medicaid and 340B programs cap reimbursement. So they cut corners. They delay maintenance. They skip audits. It’s a vicious cycle.
What’s Changing-and What Could Help
There are signs of progress. In 2022, the Department of Health and Human Services created a new role: the Supply Chain Resilience and Shortage Coordinator. Their job? To connect FDA, CDC, CMS, and manufacturers to spot problems early.
The FDA is also finalizing new rules that could require manufacturers to give earlier notice of potential shortages. Early modeling suggests this could improve detection by 25%.
Long-term, experts are pushing for:
- Reforming Medicare Part B reimbursement to reward reliable manufacturers, not just the cheapest bid.
- Investing in advanced manufacturing-like continuous production lines that can switch between drugs in hours, not weeks.
- Creating a national strategic stockpile for essential generic drugs-not just emergency supplies.
These aren’t pipe dreams. They’re proven concepts from other countries. The cost of inaction? Over $1.2 billion a year spent just managing shortages. And worse-patients dying because the right drug wasn’t there.
What You Can Do Today
If you’re a clinician, pharmacist, or administrator:
- Know your hospital’s shortage protocol. If you don’t, ask for it.
- Join or start a multidisciplinary shortage response team.
- Keep a printed and digital list of approved alternatives for your most common shortages.
- Report every shortage you experience-even if it’s brief. Data matters.
- Push for better training. If your hospital doesn’t run drills, suggest it.
Medication shortages aren’t going away. But they don’t have to be chaos. With planning, communication, and data, hospitals can turn panic into preparedness. It’s not about waiting for a miracle. It’s about doing the hard work now-so patients don’t pay the price later.
What are the most common drugs in shortage right now?
As of late 2024, the most frequently短缺 drugs are generic sterile injectables: saline solution, morphine, epinephrine, propofol, vancomycin, and antibiotics like piperacillin-tazobactam. Cancer drugs like doxorubicin and etoposide also remain in short supply. These are critical for emergency care, anesthesia, and chemotherapy. The FDA’s Drug Shortage Database is updated daily and is the most reliable source for current listings.
Can I just use a different brand of the same drug?
Not always. Generic drugs are required to be bioequivalent, but in practice, differences in inactive ingredients or manufacturing processes can affect how a drug behaves-especially in sensitive populations like the elderly or critically ill. For example, one brand of epinephrine may have a different concentration or preservative than another. Always check clinical guidelines and consult your pharmacy team before switching brands, even if they’re the same generic name.
Why don’t pharmacies just order more when they see a shortage coming?
Because they often don’t know it’s coming. The U.S. system relies on voluntary manufacturer notifications, and many delays aren’t reported until the drug is already out of stock. Even when warnings are issued, many hospitals lack the budget or storage space to stockpile extra. Safety-net hospitals, in particular, operate on thin margins and can’t afford to buy 30 days’ worth of a drug that might only be short for two weeks.
Are online pharmacies a solution for patients facing shortages?
No. Online pharmacies often can’t legally sell prescription drugs without a valid prescription, and many are unregulated. During shortages, some websites sell expired, counterfeit, or mislabeled drugs at inflated prices. The FDA has issued warnings about this repeatedly. Patients should never turn to unverified online sources. Instead, work with their pharmacy or provider to find approved alternatives.
How long do medication shortages usually last?
The average shortage now lasts 9.8 months, up from 6.2 months in 2015. Oncology drugs and anesthetics often last longer-up to 14 months. Some shortages resolve in weeks if the issue is a minor production delay. Others take years if the manufacturer shuts down a facility or faces regulatory action. There’s no quick fix for deep-rooted supply chain problems.
Is there a national database I can check for current shortages?
Yes. The FDA’s Drug Shortage Database is the official, real-time source. It’s updated daily and includes details on cause, duration, alternatives, and manufacturer information. It’s publicly accessible and used by hospitals, pharmacists, and clinicians nationwide. Always verify shortages through this source before making clinical decisions.
What Comes Next?
The system won’t fix itself. But it doesn’t need a revolution-just better rules, better incentives, and better coordination. Hospitals that treat shortages like a routine risk, not a crisis, are already seeing fewer errors, less burnout, and better patient outcomes. The question isn’t whether shortages will happen again. It’s whether you’re ready for them when they do.







ATUL BHARDWAJ
December 2, 2025 AT 17:16India knows this pain. We get expired antibiotics shipped here because no one wants them at home. Same drugs, same problems. No one talks about it.
Steve World Shopping
December 3, 2025 AT 08:46The systemic pharmacoeconomic dysregulation in the U.S. is a textbook case of market failure compounded by regulatory capture. The absence of vertical integration in generic manufacturing creates a fragile Nash equilibrium where cost minimization trumps resilience. This isn’t a shortage-it’s a structural collapse waiting for the next supply chain perturbation.
Rebecca M.
December 5, 2025 AT 07:36Oh wow, a 15-page essay on how hospitals are *surprised* they can’t afford to keep people alive. What a shocker. Next you’ll tell me the sky is blue and Medicaid patients are invisible.
Arun kumar
December 5, 2025 AT 08:07bro the whole system is just broken like a wifi router that keeps disconnecting. one plant in hyderabad messes up and half the usa is stuck with saline in a bag on the floor. why cant we just make more? oh right-money. sad.
Zed theMartian
December 5, 2025 AT 22:40Of course you’re recommending ‘simulations’ and ‘printed lists.’ How quaint. While you’re busy color-coding your emergency drug binders, the real solution is abolishing the FDA’s archaic approval process and letting the free market decide who lives and who dies. Maybe then we’d stop treating healthcare like a bureaucratic bingo game.
Ella van Rij
December 7, 2025 AT 02:23So… we’re supposed to trust the FDA’s database? The same one that took 3 weeks to flag the contaminated heparin? Yeah. Sure. I’ll just print that out and tape it to my ICU wall next to my expired CPR card.
Lynn Steiner
December 7, 2025 AT 21:01I lost my dad because they ran out of morphine. They gave him something else. He screamed for 4 hours. No one knew how to dose it. I still hear him. Why does this keep happening? Why? Why? Why? 😭
Alicia Marks
December 8, 2025 AT 03:53You’re not alone. Start a team. Talk to your pharmacy. Share the list. Small steps save lives. You’ve got this.
Paul Keller
December 8, 2025 AT 21:00While the immediate tactical responses-buffer stock, multidisciplinary teams, simulation drills-are commendable, they represent symptomatic relief rather than curative intervention. The underlying pathology lies in the commodification of essential medicines, wherein the profit motive systematically undermines public health infrastructure. A paradigm shift is required: from reactive triage to proactive sovereignty over critical pharmaceutical production. This necessitates federal investment in domestic manufacturing capacity, coupled with price floors that ensure sustainability without incentivizing monopolistic behavior. The current model is not merely inefficient-it is ethically indefensible.
Shannara Jenkins
December 9, 2025 AT 00:55My hospital started doing monthly shortage huddles last year. We didn’t fix everything-but we stopped one kid from getting the wrong dose of epinephrine because we’d practiced it. It’s not glamorous. But it works. Keep showing up.
Elizabeth Grace
December 10, 2025 AT 18:04my coworker just told me we’re out of propofol again. so now we’re using ketamine and pretending it’s chill. we’re not chill. we’re exhausted. and the patients? they’re just… waiting.