Rhabdomyolysis Medication Interaction Checker
This tool checks for dangerous medication combinations that may cause rhabdomyolysis (muscle breakdown). It is for educational purposes only and should not replace professional medical advice.
Imagine taking your daily statin for cholesterol, then adding an antibiotic for a sinus infection-only to wake up two days later with dark urine, sore muscles, and feeling like you’ve been hit by a truck. This isn’t rare. It’s a preventable medical emergency called rhabdomyolysis, and it’s happening more often than most doctors realize.
What Exactly Is Rhabdomyolysis?
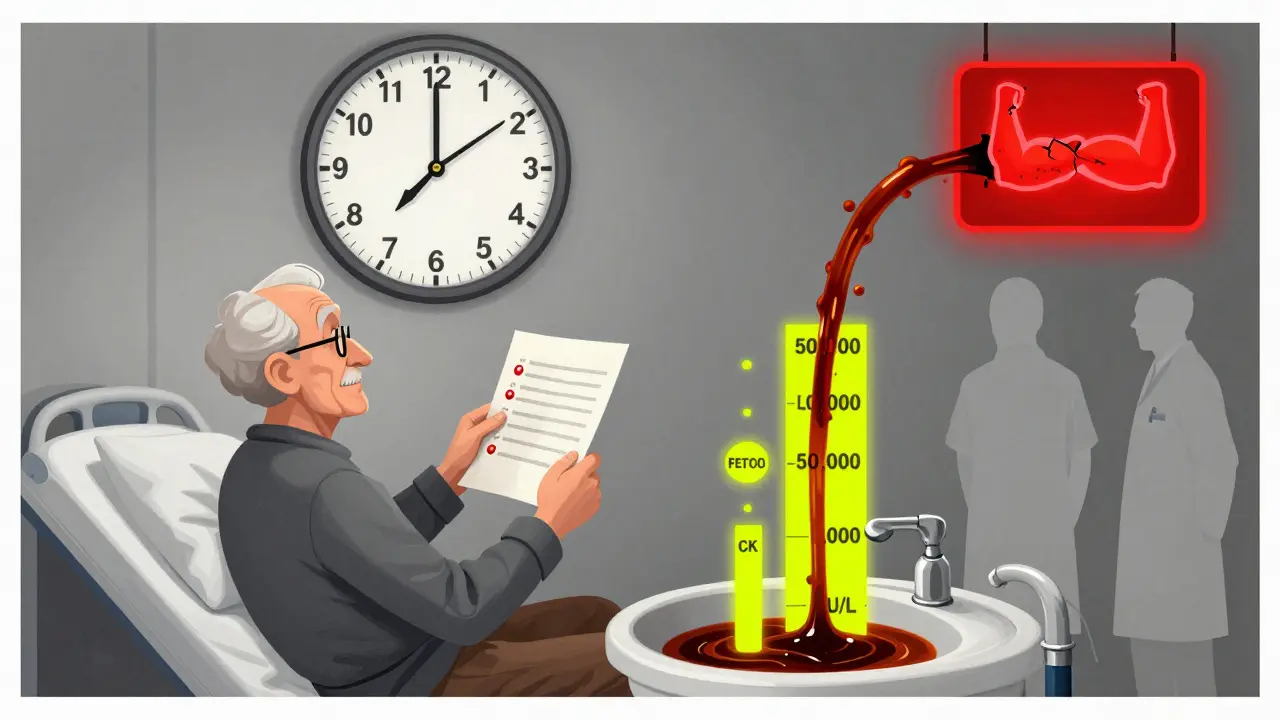
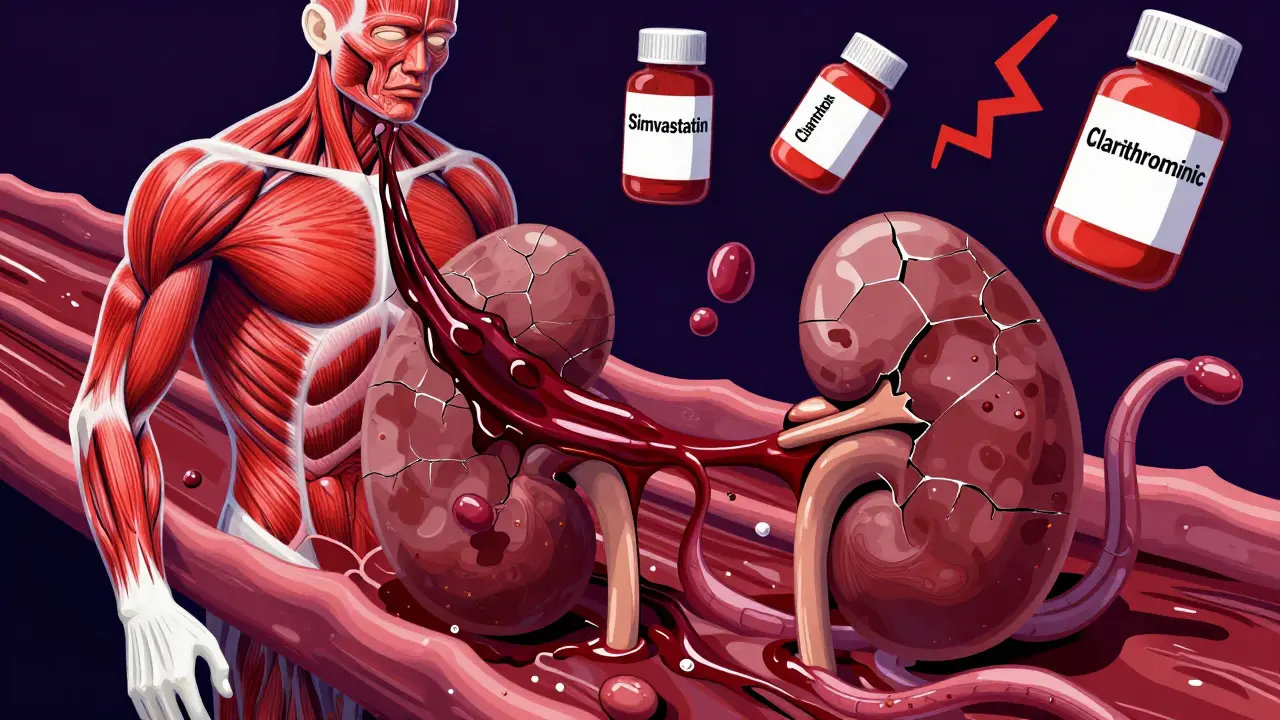
Rhabdomyolysis isn’t just muscle soreness. It’s when muscle cells break down so fast that their contents flood into your bloodstream. The worst part? One of those contents-myoglobin-can wreck your kidneys. When muscle fibers rupture, they release creatine kinase (CK), potassium, phosphate, and myoglobin. CK levels above 1,000 U/L are a red flag. In severe cases, they spike past 50,000 or even 100,000 U/L. That’s not normal muscle fatigue. That’s tissue destruction.Only about half of people with rhabdomyolysis show the classic triad: muscle pain, weakness, and dark, cola-colored urine. The rest? They might just feel nauseous, have a fever, or notice they’re peeing less. That’s why it’s often missed-until it’s too late.
Medications Are the Leading Cause
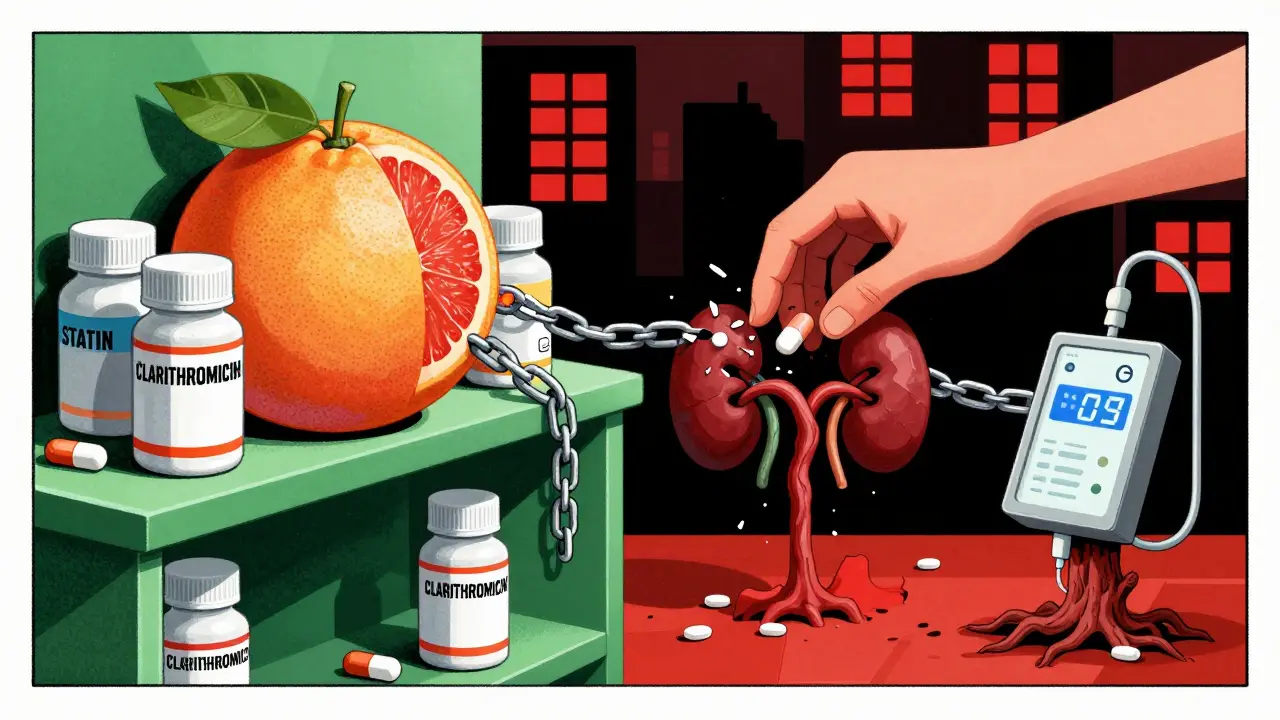
While crush injuries and extreme exercise can trigger rhabdomyolysis, today’s biggest threat comes from drug interactions. About 7-10% of all cases are caused by medications, and statins alone account for 60% of those. Atorvastatin and simvastatin are the worst offenders. But here’s the kicker: most cases don’t happen with statins alone. They happen when statins mix with other drugs.Take simvastatin and gemfibrozil together. That combo increases rhabdomyolysis risk by 15 to 20 times. Why? Both drugs are processed by the same liver enzyme-CYP3A4. When one blocks it, the other builds up to toxic levels. Same thing happens with clarithromycin, itraconazole, or even grapefruit juice. A single dose of clarithromycin can turn a safe statin dose into a life-threatening one.
It’s not just statins. Colchicine for gout? Safe alone. But combine it with clarithromycin, and rhabdomyolysis risk jumps 14-fold. Antiretrovirals like zidovudine? Up to 12% of users show CK levels more than 10 times normal. Even cancer drugs like erlotinib can trigger CK spikes over 20,000 U/L when paired with simvastatin. And propofol, used in ICUs? It shuts down mitochondrial energy production in muscle cells-leading to one of the deadliest forms, with a 68% death rate when rhabdomyolysis kicks in.
Who’s at Highest Risk?
It’s not random. Certain people are sitting ducks for this. If you’re over 65, your risk is more than three times higher. Women are 1.7 times more likely than men to develop it. If you have kidney problems-eGFR under 60-you’re 4.5 times more vulnerable. And if you’re taking five or more medications? Your risk skyrockets by 17 times.Genetics play a role too. About 1 in 5 Europeans carry the SLCO1B1*5 gene variant, which makes them far more sensitive to statin toxicity. Most doctors don’t test for it. They assume the patient is fine because they’ve been on the drug for years. But a new interaction-say, starting an antifungal for athlete’s foot-can suddenly turn that long-term statin into a time bomb.
How It Hits the Kidneys
Myoglobin is the silent killer. When it floods the blood, the kidneys try to filter it out. But myoglobin clogs the tiny tubules, causing acute kidney injury. In up to 50% of rhabdomyolysis cases, patients need dialysis. The National Registry of Drug-Induced Acute Kidney Injury reports mortality rates of 5-15% in those who develop kidney failure. That’s not a small number. That’s one in seven people dying from a preventable drug interaction.And it’s not just the kidneys. High potassium levels can trigger deadly heart rhythms. Low calcium can cause seizures or muscle spasms. In 5% of severe cases, pressure builds in the muscles themselves-compartment syndrome-requiring emergency surgery to cut open the tissue and save the limb.
When Does It Happen?
Timing matters. More than half of drug-induced cases show up within 30 days of starting a new medication or changing a dose. Statin-related cases usually appear around 28 days in. That’s why many patients think, “It’s been months-I’m fine.” But if you add a new pill, even a harmless-seeming one, your body might not handle the combo.Real patient stories confirm this. One man on colchicine for gout added clarithromycin for a cough. Within 48 hours, his urine turned dark. His CK hit 28,500 U/L. Another, on simvastatin and erlotinib for lung cancer, ended up on dialysis after his CK peaked at 42,000. Neither doctor warned them about the interaction.
What Should You Do If You Suspect It?
If you’re on any of these drugs and suddenly feel unusually weak, have dark urine, or unexplained muscle pain, stop the new medication and get to a hospital. Don’t wait. Don’t call your doctor tomorrow. Go now.Doctors diagnose it with a simple blood test: creatine kinase. If it’s over 1,000 U/L and you’re on a risky combo, rhabdomyolysis is likely. Treatment is aggressive: at least 3 liters of IV fluids in the first 6 hours, followed by continuous hydration to keep your urine flowing at 200-300 mL per hour. Alkalinizing the urine with sodium bicarbonate helps prevent myoglobin from clumping in the kidneys.
Some cases need plasma exchange-especially if you’re on leflunomide, a drug for rheumatoid arthritis with a 2-week half-life. That means it sticks around for weeks. Plasma exchange can remove it faster than your liver can.
What Doctors Should Be Doing
The American Society of Nephrology says drug-induced rhabdomyolysis makes up 5-7% of all acute kidney injury cases in hospitals. Yet, most providers still don’t screen for it. The FDA and EMA have issued warnings. EMA now requires all statin labels to list specific contraindications with CYP3A4 inhibitors. But warnings on a label don’t help if the prescriber doesn’t check.There’s a gap between guidelines and practice. A 2022 Reddit analysis of 147 cases found 92% of patients said their provider didn’t recognize early muscle symptoms as dangerous. That’s not just negligence-it’s systemic.
Doctors need to ask: What else is this patient taking? Not just prescriptions-supplements, OTC meds, even herbal teas. A single dose of itraconazole for toenail fungus can be enough to trigger a crisis in someone on simvastatin.
The Bigger Picture
In 2020, the U.S. saw over 27,000 hospitalizations for drug-induced rhabdomyolysis. Each one cost an average of $28,743. That’s more than $780 million a year in avoidable costs. And the problem is growing. With aging populations and rising polypharmacy, incidence could climb 8.2% per year through 2030.Research is moving forward. The NIH is funding a real-time drug interaction alert system. Genetic testing for SLCO1B1*5 is becoming more accessible. New drugs are being tested to protect mitochondria from statin damage. But until those tools are in every clinic, the burden falls on patients and providers to be vigilant.
What You Can Do Right Now
If you’re on a statin, colchicine, or any chronic medication:- Know your drugs. Write down every pill you take-prescription, OTC, supplement.
- Ask your pharmacist: “Could any of these interact to cause muscle damage?”
- If you start a new drug, watch for muscle pain, weakness, or dark urine for the first 30 days.
- Don’t assume “it’s been years, so it’s safe.” Interactions can happen at any time.
- If you’re over 65, have kidney issues, or take five or more meds-be extra cautious.
There’s no shame in asking questions. Your life might depend on it.
Can rhabdomyolysis happen even if I’ve been on my medication for years?
Yes. Rhabdomyolysis often occurs after adding a new drug, not after long-term use alone. For example, someone on simvastatin for five years may be fine-until they start clarithromycin for a sinus infection. The interaction suddenly raises statin levels to toxic levels, triggering muscle breakdown. Timing matters more than duration.
Are all statins equally risky for rhabdomyolysis?
No. Simvastatin and lovastatin are the most likely to cause problems because they’re heavily processed by the CYP3A4 enzyme. Atorvastatin carries moderate risk. Pravastatin and rosuvastatin are much safer because they’re cleared differently. If you’re on a high-risk statin and need an antibiotic or antifungal, ask your doctor if switching to pravastatin or rosuvastatin is an option.
Is dark urine always a sign of rhabdomyolysis?
Not always, but it’s a major red flag. Dark, cola-colored urine can also come from dehydration, intense exercise, or certain foods like beets. But if you’re on medications known to cause muscle breakdown-like statins, colchicine, or antivirals-and your urine turns dark, don’t wait. Get a creatine kinase test immediately. Delaying can mean kidney failure.
Can I take over-the-counter painkillers if I’m on a statin?
Most OTC painkillers like acetaminophen (Tylenol) are safe. But NSAIDs like ibuprofen or naproxen can stress the kidneys, especially if you already have early muscle breakdown. If you’re feeling unusually sore or have dark urine, avoid NSAIDs until you’re cleared by a doctor. The combination can worsen kidney injury.
How long does recovery take after rhabdomyolysis?
Recovery varies. If your kidneys weren’t damaged, most people recover muscle strength in about 12 weeks. But if you needed dialysis, recovery can take over 6 months. And 44% of survivors still report muscle weakness six months later. Full recovery isn’t guaranteed-even if you survive.
Should I get genetic testing for SLCO1B1*5 before starting a statin?
It’s not routine yet, but if you’re over 65, have a family history of statin side effects, or need a high-dose statin, it’s worth asking. The SLCO1B1*5 gene increases simvastatin toxicity risk by 4.5 times. If you carry it, your doctor can choose a safer statin or lower the dose. Some clinics now offer this test as part of pre-prescription screening.
Drug interactions don’t always come with warning labels. Sometimes, the only warning is your body screaming in pain. Know the risks. Ask the questions. Your muscles-and your kidneys-depend on it.






Beth Cooper
January 31, 2026 AT 09:54Okay but have you ever heard of the real reason this is happening? Big Pharma doesn't want you to know that statins were originally designed as a fungicide and they're basically poisoning your mitochondria on purpose. They're making billions while you're on dialysis. The FDA? Totally bought out. I've seen the leaked emails. You think your doctor's helping you? Nah. They're just following the script.
Katie and Nathan Milburn
February 1, 2026 AT 21:01It is of considerable importance to note that the pharmacokinetic interactions delineated herein represent a well-documented, clinically significant phenomenon, particularly with regard to the cytochrome P450 3A4 isoenzyme pathway. The elevated risk of rhabdomyolysis in polypharmacy patients is not merely anecdotal but substantiated by multiple peer-reviewed meta-analyses, including those published in the Journal of Clinical Pharmacology and the American Journal of Kidney Diseases.
Marc Bains
February 1, 2026 AT 23:24Listen, I’ve seen this happen in my clinic. Grandmas on statins, adding a new antibiotic because they got a cold - boom, next week they’re in the ER. We need to stop treating patients like they’re just a list of meds. Talk to them. Ask what else they’re taking - even that ‘natural’ supplement from the health food store. And for God’s sake, stop assuming ‘they’ve been on it for years so it’s fine.’ That’s how people end up losing kidneys. We’ve got to do better.
kate jones
February 2, 2026 AT 01:59The clinical presentation of drug-induced rhabdomyolysis is often insidious, characterized by subacute myalgia, myoglobinuria, and a disproportionate elevation in serum creatine kinase (CK) levels - typically exceeding 1,000 U/L, with severe cases surpassing 50,000 U/L. The pathophysiological cascade involves mitochondrial dysfunction, calcium-mediated proteolysis, and tubular obstruction secondary to myoglobin precipitation. Early aggressive hydration with isotonic saline, coupled with urinary alkalinization (target pH >6.5), remains the cornerstone of management. Genetic polymorphisms in SLCO1B1 significantly modulate statin uptake into hepatocytes, increasing systemic exposure and subsequent myotoxicity.
Natasha Plebani
February 2, 2026 AT 10:33There’s something deeply ironic about how we’ve turned medicine into a mathematical equation - dosage x drug x gene = outcome - while ignoring the existential reality that our bodies are not machines. We treat statins like they’re just another ingredient in a recipe, but muscle isn’t a widget. It’s living tissue, shaped by centuries of evolution, and when we force it into a metabolic bottleneck with a cocktail of synthetic compounds, we’re not just risking kidney failure - we’re violating a kind of biological dignity. Maybe the real question isn’t ‘how do we prevent this?’ but ‘why do we keep doing this to ourselves?’
Yanaton Whittaker
February 4, 2026 AT 08:20AMERICA IS GETTING WEAK! We’re so scared of a little muscle pain we’re giving up our meds like it’s a cult! Back in my day, you took your pills, you worked through the soreness, and you didn’t whine to your doctor every time you felt tired! This is why we’re losing to China - too many people think their body’s a fragile doll! 🇺🇸💪
Carolyn Whitehead
February 4, 2026 AT 16:51I just started a new med last month and I’ve been feeling a bit off but thought it was stress. Now I’m gonna check my urine color and write down everything I take. Thanks for the nudge - I’m glad I read this before something bad happened 😊
Amy Insalaco
February 6, 2026 AT 02:58It’s fascinating how the medical establishment has managed to pathologize the natural metabolic consequences of pharmaceutical polypharmacy under the banner of ‘preventive care.’ The statin paradigm, in particular, represents a triumph of pharmacoeconomic ideology over physiological epistemology. The very notion that lowering LDL cholesterol via HMG-CoA reductase inhibition confers a net survival benefit in primary prevention is statistically dubious at best - and the rhabdomyolysis crisis is merely the most visceral manifestation of a broader epistemic collapse in clinical medicine. We’ve replaced wisdom with algorithmic prescribing.
Kimberly Reker
February 7, 2026 AT 10:43You’re not alone if you’re scared. I was too. But now I keep a little med log on my phone - every pill, every supplement, even the turmeric I sneak in my tea. And I ask my pharmacist every time something new shows up. It’s not hard. It’s just something nobody teaches you. You’ve got this. And if you’re feeling weird? Go get checked. Better safe than sorry - your muscles will thank you ❤️
Sarah Blevins
February 8, 2026 AT 18:48While the article presents a compelling narrative, it lacks a critical analysis of confounding variables such as comorbidities, adherence rates, and the prevalence of illicit substance use in the cohort. The statistical correlations cited do not establish causality, and the anecdotal evidence presented may be subject to selection bias. Furthermore, the assertion that ‘doctors don’t recognize early symptoms’ is unsupported by longitudinal clinical audit data.
Kathleen Riley
February 9, 2026 AT 21:42One cannot help but reflect upon the ontological dissonance inherent in modern pharmacotherapy: the pursuit of longevity through chemical intervention, while simultaneously undermining the very biological substrate that sustains life. Rhabdomyolysis, then, is not merely a side effect - it is a metaphysical protest of the flesh against the tyranny of the pill. The body remembers what the algorithm forgets.
Donna Fleetwood
February 11, 2026 AT 17:20My dad had this happen after he started an antifungal cream and didn’t tell his doctor. He was fine for years on simvastatin - then boom. He’s okay now, but he had to get dialysis for a week. He says he’ll never skip the ‘what else are you taking?’ question again. If you’re on meds, talk to someone. Seriously. It’s not scary, it’s smart.
Melissa Cogswell
February 13, 2026 AT 05:01Just wanted to add - if you’re on statins and take colchicine for gout, ask your pharmacist about the CYP3A4 interaction. My rheumatologist didn’t mention it, but my pharmacist caught it when I asked. Switched me to febuxostat. No more muscle pain. Small question, big save.